By Mike Darwin
 Contemporary Medicine: Playing Peek-a-Boo with Death
Contemporary Medicine: Playing Peek-a-Boo with Death
The Proper End of Medicine
In my experience, physicians get evaluations that parallel those most often given to prostitutes; they don’t pay enough attention to you, there is typically a lack of the desired amount of enthusiasm and intimacy, the critical emotional moments are faked, the encounter never lasts long enough, you may discover as a consequence of your visit that you have a loathsome disease, the hourly rate is punishing, and the most you can hope for is palliation, not real relief.
The first thing that anyone needs to understand about medicine is what its proper goal is. That’s actually pretty simple: to cure disease and maintain good health. No further qualifications are necessary. Once that proposition is accepted, it then should become obvious that the end goal, and the ultimate ideal of medicine, is to keep people alive and in good health indefinitely. Even the television physician pundits, like Dr. Oz, and CNN’s Sanjay Gupta, can sense that this is coming, and in fact, Sanjay pretty much said so:
“Practical immortality may now be within our grasp thanks to the cutting-edge scientific research and amazing medical breakthroughs that are coming at such astonishing speed we can hardly keep up. “1
- Sanjay Gupta, M.D.
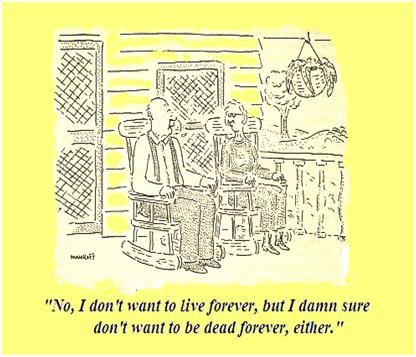 Figure 1: Immortality is a lot like sex, in that it is something few will admit to wanting a lot of, and that almost everyone thinks their neighbor has too much of.
Figure 1: Immortality is a lot like sex, in that it is something few will admit to wanting a lot of, and that almost everyone thinks their neighbor has too much of.
So, despite the fact that most people, when asked, will recoil in horror from the notion of personal, biological immortality, the fact is that that is exactly what they expect, exactly what they want, and exactly what they will effectively demand. Unfortunately, most of the medicine we practice today is not only not going to provide immortality any time soon, it is going to bankrupt us while turning us into human fleshpots, sitting in the solariums of nursing homes and extended care facilities the world over.
The late great physician-philosopher-writer Lewis Thomas, first identified the problem in 1974, in his classic book, The Lives of a Cell. Thomas wrote insightfully about three different kinds of medicine we humans are capable of practicing, classifying them as Prevention, No Technology, Low Technology, Halfway Technology and High Technology. I have created a color wheel of Thomas’ medical technologies, and added one of my own: Futile Technology – the kind of technology which increasingly characterizes the medicine we practice today (Figure 2).
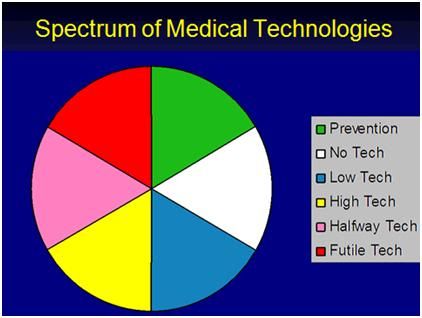
Figure 2: The Spectrum of current medical technologies practiced today
Prevention and low technology medicine are fairly straightforward concepts and do not need our attention here. But High Technology Medicine (HTM), Futile Technology (FT), and especially Halfway Technology (HT), deserve considerably greater scrutiny.
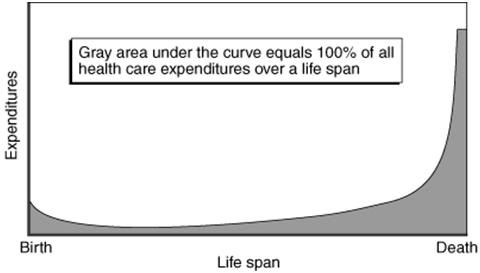 Figure 3: The distribution of heal care expenditures over a lifetime: most of the money is spent on the last decade of life and most of that on futile and ineffective medicine that turns dying into a long, costly, morbid process. Nation-states would do better to advise their citizens to smoke and drink with abandon if they are truly interested in reducing the amount of suffering, and avoiding bankrupting their entire economies. Alternatively…
Figure 3: The distribution of heal care expenditures over a lifetime: most of the money is spent on the last decade of life and most of that on futile and ineffective medicine that turns dying into a long, costly, morbid process. Nation-states would do better to advise their citizens to smoke and drink with abandon if they are truly interested in reducing the amount of suffering, and avoiding bankrupting their entire economies. Alternatively…
Thomas elegantly describes Halfway Technology as follows:
“Halfway technology represents the kinds of things that must be done after the fact, in efforts to compensate for the incapacitating effects of certain diseases whose course one is unable to do very much about. By its nature, it is at the same time highly sophisticated and profoundly primitive… It is characteristic of this kind of technology that it costs an enormous amount of money and requires a continuing expansion of hospital facilities… It is when physicians are bogged down by their incomplete technologies, by the innumerable things they are obliged to do in medicine, when they lack a clear understanding of disease mechanisms, that the deficiencies of the health-care system are most conspicuous… The only thing that can move medicine away from this level of technology is new information, and the only imaginable source of this information is research. The real high technology of medicine comes as the result of a genuine understanding of disease mechanisms and when it becomes available, it is relatively inexpensive, relatively simple, and relatively easy to deliver.” —Lewis Thomas2
 Figure 4: Polio victims on Iron Lung support in a school gymnasium in the mid-1950s.
Figure 4: Polio victims on Iron Lung support in a school gymnasium in the mid-1950s.
To understand the difference between HT and High Technology medicine (HTM), Thomas used the paradigm of the Polio epidemics of the mid-20th century as an example.3 Today, very few people understand either what the Polio epidemics of the 1950s were like, or the divergent ways that both researchers and clinicians sought to address the scourge. On the one hand, hundreds of thousands of people were contracting polio, with many suffering irreversible bulbar paralysis; which meant that they were unable to breathe. They were conscious and very much alive, but they were unable to use their respiratory muscles to ventilate themselves.
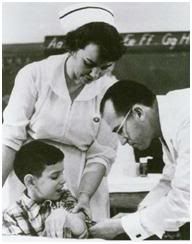 Figure 5: Jonas Salk, discoverer of the first clinically deployed Polio vaccine.
Figure 5: Jonas Salk, discoverer of the first clinically deployed Polio vaccine.
For many of such paralyzed patients, a relatively new medical device in the form of the Iron Lung represented an opportunity to go on living. In some patients the paralysis retreated, or vigorous physical therapy allowed them to recover sufficiently that they could once again breathe on their own.4 But for many, the Iron Lung was a life sentence of paralyzed immobility inside a cylindrical ‘steel coffin’ as seen in Figure 4.
A minority of scientists at that time believed that it might be possible to defeat Polio by the expedient of a vaccine,5 and so an intense competition for funds began between those who sought to secure more Iron Lungs to support the ever growing legion of patients with respiratory paralysis, and those who sought to understand the fundamental basis of the disease (in the context of their technological era) and treat it by eliminating it.6 In other words, these researchers wanted to get to the root cause of the illness and stop it there, rather than to develop every more sophisticated Iron Lungs, and other prostheses, to pinch-hit for the muscles rendered useless and atrophied by Polio.
In one of the most rapid translation of bench research to bedside application, Jonas Salk and his colleagues developed a workable Polio vaccine7 which was rolled out for public use in 1955 – the year I was born – just in time to ensure that yours truly would not end up in an Iron Lung, or be ‘lucky’ enough to escape a brush with Polio confined to wheelchair, or using walking braces with a case of ‘simple paralysis,’ as did US President Franklin Delano Roosevelt. HT is Iron Lungs, and the Salk, and later Sabin vaccines, were HTM. Insulin treatment for diabetes, artificial hearts/ left ventricular assist devices, total hip and knee replacements, and drugs for hypertension are also all halfway medicine. They treat the clinical manifestations of disease with varying degrees of efficiency and cost effectiveness, but they do not ever affect a cure.
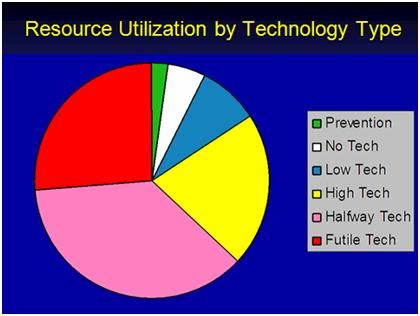 Figure 6: The chart above shows the approximate current distribution of health care dollars by the type of medical technology.
Figure 6: The chart above shows the approximate current distribution of health care dollars by the type of medical technology.
Most people aren’t satisfied with medicine because, fundamentally, most of medicine is still unable to address the underlying causes of disease. Medicine used to be almost completely worthless from a scientific standpoint, and physicians were mostly about diagnosis, prognosis, and hand-holding. Since 1900, medicine has been able to treat a few illnesses definitively, but it is still mostly about indirect, and halfway treatments that are costly, and in no way definitive. The older the patient, the more this will be the case, because the real cause of most disease in the developed world is aging. Cancer is aging, hypertension is aging, diabetes is aging, most of urology (including sexual dysfunction) is aging, stroke is aging, Alzheimer’s is aging, and 3/4ths of every health care dollar is currently spent on the deterioration and chronic illnesses that are a product of aging.
Patient’s don’t have the experience of their physicians examining them, and then saying, “Well, you see, the problem is right here in alpha-N-1-letterbox beta gene. I’ve re-coded that gene, as well added on the 5.01 Rejuvenation and Cell Repair Package. Within 10 days to two weeks, you should have the libido of a 14-year-old, the appearance of a 20-year-old, the stamina of an endurance runner, and the life span of a Sequoia redwood.” Doctors can only very indirectly manipulate the machinery that makes us run, and they usually have to use costly and chronically applied chemicals that are typically as poisonous as they are therapeutic. Nobody is truly going to be thrilled about doctors until they can really cure illnesses.
 Figure 7: This is as good as it gets. If contemporary medicine reached it goal of ‘squaring the curve,’ and extending the average life span to at or near the maximum lifespan (~ 120 years), this is how you can expect to end up. The photo at left is of ‘Supercentenarian’ Marie Bremont, taken on her 115th birthday in 2001. Absent definitive regenerative medicine, all that contemporary medical technology can do is to maintain the function of existing tissues, until the point where physiological reserves become so depleted, that the slightest environmental challenge causes death.
Figure 7: This is as good as it gets. If contemporary medicine reached it goal of ‘squaring the curve,’ and extending the average life span to at or near the maximum lifespan (~ 120 years), this is how you can expect to end up. The photo at left is of ‘Supercentenarian’ Marie Bremont, taken on her 115th birthday in 2001. Absent definitive regenerative medicine, all that contemporary medical technology can do is to maintain the function of existing tissues, until the point where physiological reserves become so depleted, that the slightest environmental challenge causes death.
Because medicine is mostly a halfway business, it will have a terrible bite-back effect that will ultimately render it unsustainable, and/or leave the patient population truly pissed-off. The better we get at halfway medicine, the less cost effective it is. Dialysis, total artificial hearts, Gleevec, Viagra, anti-hypertensives, artificial joints, all these things ultimately create more and more people whose survival, let alone their restoration to health or full function, will eventually cost more than they, or the society as a whole, could possibly pay for, even with a with a lifetime of hard work. In fact, right now medical care is consuming 16% of the US GDP, and that will rise to over 20% in just 4 years! No economy that we have any experience with can tolerate that kind of cash drain – it is simply unsustainable. And what’s worse, a quick glance at Figure 6 shows that currently we are spending ~25% of our health care dollars on FT – medicine which does no good, and which usually causes harm, by inflicting further suffering, and damaging the ability of the system to deliver care to patients who can genuinely benefit.
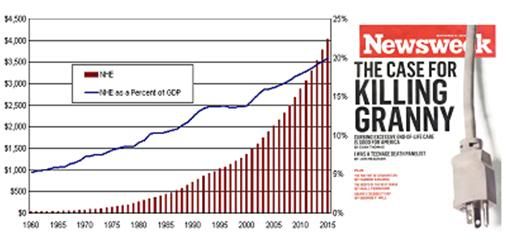
Figure 8: US healthcare costs projected to 2015 as a percentage of the GDP. The Newsweek article actually makes the case for the inevitability, and the fiscal wisdom of, “killing Granny.”8,9
So, we have only two pragmatic alternative systems:
1) Stop treating a large fraction of the population for chronic or costly illnesses and focus all our resources on diseases which can be definitively and cost-effectively managed. This sounds good, but leaves us forever trapped in a cruel world of stunted, or absent medical progress, and beset with a population suffering and dying, without hope.
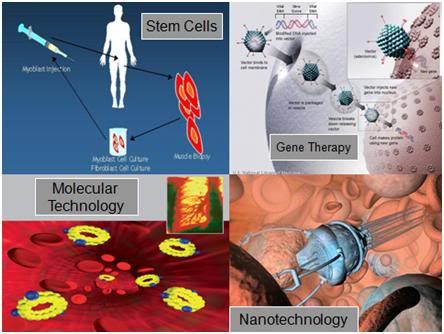 Figure 9: Some examples of definitive, curative, high technology medicine. Stem and gene cell therapy are now in the early stages of being developed, and will constitute the first wave of ‘regenerative medicine.’ If the current rate of technological progress is sustained, it seems reasonable to presume that the first autonomous cell repair technologies will begin to see laboratory application by the closing decades of this century with mature applications coming sometime in the opening decades of the 22nd century.10
Figure 9: Some examples of definitive, curative, high technology medicine. Stem and gene cell therapy are now in the early stages of being developed, and will constitute the first wave of ‘regenerative medicine.’ If the current rate of technological progress is sustained, it seems reasonable to presume that the first autonomous cell repair technologies will begin to see laboratory application by the closing decades of this century with mature applications coming sometime in the opening decades of the 22nd century.10
2) Change how we spend our money, and focus on developing definitive medicine. Definitive medicine means controlling aging and addressing and treating the cause of disease at the molecular level, where it originates.
Until we have definitive medicine (which will happen incrementally, not suddenly) we need a cost effective way to manage patients with maladies that can only be halfway treated, or not treated at all. That means we need to develop truly reversible solid state suspended animation (SA). Within the past few years, a technology has been developed that allows for deep subzero cooling of organs and tissues without any ice formation occurring. This is possible because high concentrations of cryoprotective agents – antifreeze compounds exactly like the ethylene glycol and propylene glycol used in automotive radiator antifreeze – reduce the probability of ice formation and propagation, and at high enough concentrations, these compounds can prevent ice formation completely, even at the slow cooling and warming rates that are necessary to transfer heat out of and back into and large masses of tissue, such as human organs, or human beings.11-14
Because ice formation is inhibited, further cooling of the system results in increasing viscosity until, finally, the solution becomes so viscous that it has solidified. The point at which the system makes the transition from an ultra-viscous liquid, to a molecularly arrested glass (the glass transition point, Tg), is the point at which essentially all chemical and biological activity is halted. This arrest of chemistry occurs independent of the temperature, and is a consequence of the immobilization of the chemical reactants in the glassy substrate of the cryoprotectant-water mixture. The conversion of an aqueous solution into a glass is know as vitrification, from the Latin word vitrum, which means glass.
As a result of recent advances in vitrification technology, it is now possible to vitrify entire organs.15,16 However, a significant remaining problem is to inhibit ice growth during re-warming in some tissues that do not equilibrate well with the cryoprotectant chemicals. This ice formation occurs as a result of the generation of ultramicroscopic ice nuclei during cooling, which cannot grow or propagate, because there is too little energy in the system, and too little time for ice to grow as a result of steady and continued cooling to Tg.17 While this is a significant hurdle to be overcome, it is a technological, rather than a theoretical one. Additionally, virtually all research on reversible vitrification of organs has been conducted on the kidney, and this presents a unique challenge, because the interior of the organ, the renal medulla, is very poorly circulated. It is thus difficult to load a sufficient concentration of cryoprotectants into this poorly vascularized tissue to completely avoid ice formation.
 Figure: 10: Visual appearance of ice in a rabbit kidney that was cross-sectioned during rewarming. The kidney was perfused with a cryoprotective mixture called M22 at -22°C, cut in half, immersed in M22, vitrified at -135°C, and eventually re-warmed at ~1°C/min while being periodically photographed. Times (1:30 and 1:40) represent times in hours and minutes fom the start of slow warming. The temperatures refer to ambient atmospheric temperatures near the kidney but not within the kidney itself. The upper panel shows the kidney at the point of maximum ice cross-sectional area, and the lower panel shows the kidney after complete ice melting. Both panels show the site of an inner medullary biopsy taken for differential scanning calorimetery in order to determine the actual concentration of cryoprotectants in the tissue with high precision. [http://cryoeuro.eu:8080/download/attachments/425990/FahyPhysicBiolAspectsRenalVitri2010.pdf?version=1&modificationDate=1285892563927]
Figure: 10: Visual appearance of ice in a rabbit kidney that was cross-sectioned during rewarming. The kidney was perfused with a cryoprotective mixture called M22 at -22°C, cut in half, immersed in M22, vitrified at -135°C, and eventually re-warmed at ~1°C/min while being periodically photographed. Times (1:30 and 1:40) represent times in hours and minutes fom the start of slow warming. The temperatures refer to ambient atmospheric temperatures near the kidney but not within the kidney itself. The upper panel shows the kidney at the point of maximum ice cross-sectional area, and the lower panel shows the kidney after complete ice melting. Both panels show the site of an inner medullary biopsy taken for differential scanning calorimetery in order to determine the actual concentration of cryoprotectants in the tissue with high precision. [http://cryoeuro.eu:8080/download/attachments/425990/FahyPhysicBiolAspectsRenalVitri2010.pdf?version=1&modificationDate=1285892563927]
A fair summary of the current technological state of the art is that it is likely now possible to place complex mammalian organs, such as the rabbit kidney, into indefinitely long suspended animation, with little or no loss of viability, and no damage as a consequence of structural disruption due to ice formation. The use of radio frequency, or microwave illumination to speed rewarming, the use of warm gas (such as helium) to perfuse the organ’s circulation, or a combination of both, may offer a workable solution to the problem of ice formation during rewarming. The point is, we are now palpably close to a fully reversible technology for inducing suspended animation in complex living systems. Perhaps most impressively, one mammalian kidney has survived vitrification and rewarming sufficiently intact to permit immediate support of the rabbit from which it was removed (as the sole kidney), until the animal was sacrificed for evaluation 29 days after the organ was re-implanted.
SA brings the cost of caring for any patient down to ~$1K dollars per year, and accomplishes something that most people find very satisfying in life; namely giving their intractable problems to someone else to solve. Since we are already sending our bills for our health care to the future, it only seems reasonable that we should send ourselves along, too. Figure11: The first kidney to survive vitrification shortly before it was removed from the animal for evaluation after supporting its life as the sole kidney for 29 days.
Figure11: The first kidney to survive vitrification shortly before it was removed from the animal for evaluation after supporting its life as the sole kidney for 29 days.
The problem of aging will be a difficult one to solve, and answers will come in iterations that unfold over the remaining decades of this century (providing we make this problem a priority – or survive as a technological civilization). While no well informed scientist would argue that controlling (and even reversing) senescence is impossible, or even unlikely before the turn of the century, no responsible scientist would argue that we understand aging in the way the Wright Brothers did flight at the dawn of the last century. There is a huge difference between a technological problem, and a theoretical problem. Flight in 1907 was a technological problem, as was interplanetary rocketry in 1937: the theory was there, but the technology wasn’t.
 Figure 12: The first sustained heavier-than-air human flight, on 17 December, 1903.
Figure 12: The first sustained heavier-than-air human flight, on 17 December, 1903.
Today, with respect to suspended animation, we are more or less exactly where Orville and Wilbur Wright found themselves after they first achieved sustained heavier-than-air human flight, on 17 December, 1903, and where Goddard and Von Braun were in 1937 in terms of achieving space travel. We now have a full understanding of the theoretical requirements for suspended animation, we have a solid proof of principle (mammalian organs have recently been reversibly cryopreserved), and what remains to be done is to develop and expand the technology. Once medicine has SA, it has a cost effective means to offer the promise of definitive therapy to almost every dying patient, at a fraction of the cost currently expended to deliver futile, halfway, or custodial care.
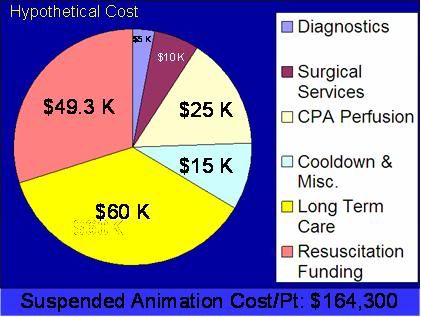 Figure 13: A rough estimate of the cost for induction of suspended animation in humans, followed by indefinite maintenance at ~135oC until such time as definitive medical treatment, including mature regenerative medicine to treat aging, becomes possible. (Estimate prepared by the author using current costs of cryonic cryopreservation at the Alcor Life Extension Foundation in Phoenix, AZ; with assumed reduction in costs as a result of economies of scale in long-term cryogenic care).
Figure 13: A rough estimate of the cost for induction of suspended animation in humans, followed by indefinite maintenance at ~135oC until such time as definitive medical treatment, including mature regenerative medicine to treat aging, becomes possible. (Estimate prepared by the author using current costs of cryonic cryopreservation at the Alcor Life Extension Foundation in Phoenix, AZ; with assumed reduction in costs as a result of economies of scale in long-term cryogenic care).
Physicians, politicians, bioethicists – they are all confronted with a looming practical and moral catastrophe, and a difficult choice to make. It would appear that the reasonable and humane choice is to fund and perfect the only research that offers the prospect of indefinitely stabilizing care to virtually all dying patients: reversible human suspended animation. That is the most pragmatic, humane and cost effective solution to the inadequacy of, and the problem of, universal health care. Quality, satisfying, universal health care coverage is eminently affordable, indeed it is a trivial societal expense the instant halfway, futile, end of life, and custodial care are subtracted from the package. We can do that humanely with SA, or inhumanely with restrictions on care. There really isn’t any middle ground.

References
1) Gupta, S. Cheating Death. Grand Central Publishing 2009. ISBN: 044650887X
2) Thomas L. The technology of medicine. In: The Lives of a Cell. New York, NY: Viking Press; 1974:31–36.
3) Silver, JK, Wilson, DJ. Polio Voices. Santa Barbara: Praeger Publishers. 2007 p. 141.
4) Wilson DJ. And they shall walk: ideal versus reality in polio rehabilitation in the United States. Asclepio. 2009;61(1):175-92.)
5) Smith, JS. Patenting the Sun: Polio and the Salk Vaccine. William Morrow & Co; 1st edition. 1990. ISBN-10: 0688094945.
6) Juskewitch JE, Tapia CJ, Windebank AJ. Lessons from the Salk polio vaccine: methods for and risks of rapid translation. Clin Transl Sci. 2010;3(4):182-5.
7) Bookchin, D, Schumacher, J. The Virus and the Vaccine, Macmillan, 2004. ISBN 0312342721.
8) Office of the Actuary in the Centers for Medicare & Medicaid Services annually produces projections of health care spending for categories within the National Health Expenditure Accounts, National Health Expenditure Projections 2009-2019: http://www.cms.gov/NationalHealthExpendData/downloads/NHEProjections2009to2019.pdf.
9) Chernew, ME, Baicker, K, Hsu, J.The Specter of Financial Armageddon — Health Care and Federal Debt in the United States. NEJM (10.1056/NEJMp1002873) was published on March 17, 2010, at NEJM.org. http://healthpolicyandreform.nejm.org/?p=3170. Retrieved December 23, 2010.)
10) Freitas, R. Nanomedicine. 1999: http://www.nanomedicine.com/NMI.htm.
11) Fahy, GM, Wowk, B, Wu J. Cryopreservation of complex systems: the missing link in the regenerative medicinesupply chain. Rejuvenation Res. 2006; 9:279-91.
12) Wowk, B, Fahy GM. Toward large organ vitrification: extremely low critical cooling and warming rates of M22 vitrification solution. Cryobiology. 2005; 51:362.
13) Wowk B, Fahy GM. Ice nucleation and growth in concentrated vitrification solutions. Cryobiology. 2007; 330.
13) Wowk, B, Thermodynamic aspects of vitrification. Cryobiology 2010; 60(1):11-22.
14) Fahy GM. Vitrification: An overview. In: Liebermann J, Tucker MJ, eds. Vitrification in Assisted Reproduction: A User’s Manual and Troubleshooting Guide. London: Informa Healthcare 2007; (in press).
15) Fahy GM, Wowk B, Wu J, Paynter S. Improved vitrification solutions based on predictability of vitrification solution toxicity. Cryobiology 2004; 48:22-35: http://cryoeuro.eu:8080/download/attachments/425990/FahyImprovedVitriSolns2004.pdf?version=1&modificationDate=1285892436630
16) Fahy, GM, Wowk, B, Pagotan, R, et al. Physical and biological aspects of renal vitrification. Organogenesis 2009; 5:3, 167-175: http://cryoeuro.eu:8080/download/attachments/425990/FahyPhysicBiolAspectsRenalVitri2010.pdf?version=1&modificationDate=1285892563927
17) Fahy GM. The role of nucleation in cryopreservation. In: Lee REJ, Warren GJ, Gusta LV, eds. Biological ice nucleation and its applications. St. Paul: APS Press 1995; 315-36.

Patrick,
You are certainly welcome to send me material on your company and its services. My particular questions would be about your physical facilities and references (business and scientific). Where are your facilities located, and are they open to public inspection/yours? i look forward to receiving material from you: m2darwin@aol.com