Calorie Restriction: First You Starve and Then You Die (Horribly)
 Figure 1: Supercentenarians in “extreme old age”: Jeane Calmette, 121; Ingeborg Mestad, 110; Walter Breuning, 114; Marie-Louise Meilleur, 117.
Figure 1: Supercentenarians in “extreme old age”: Jeane Calmette, 121; Ingeborg Mestad, 110; Walter Breuning, 114; Marie-Louise Meilleur, 117.
There’s a proven technique in animals for reaching the maximum lifespan; the longest time that animals of a given species have the inherent capacity to survive. It’s called calorie restriction, and there is a large body of animal data in an impressive range of species that says it works. There is even an ongoing project being conducted by the National Institutes of Aging (NIA) to evaluate calorie restriction in primates and it seems to be working in them, too. The calorie restricted Rhesus macaque monkeys have lower death rates, lower rates of age-associated degenerative diseases, and their overall health and activity level are dramatically better than is the case for the control animals, who are fed a diet that simulates the ad lib calorie intake by humans in the Developed World.
There’s just one catch, and that is that calorie restriction, to the extent necessary to get the individual to the maximum end of the lifespan envelope is, for most humans, a miserable experience. It is also one fraught with the potential for malnutrition and the development of eating disorders, such as anorexia nervosa and bulimia. But there’s another problem with calorie restriction in humans, and that’s that the end results are that you end up a blind, debilitated old crone or codger, and then you die.
Having said that, I don’t want to minimize or dismiss the probable very real advantages of calorie restriction in humans and they are that there is likely to be, on average, a 15-25 year extension of the healthy and reasonably productive lifespan, with a large decrease in most of quality of life eroding (and costly) degenerative diseases, such as diabetes, cardiovascular disease, osteoarthritis, dementia and very likely, tooth decay and gum disease. That’s impressive, even if it isn’t very practical for most people without some kind of pharmacological assistance.
There is also ongoing research to discover drugs that mimic the effects of calorie restriction on gene expression so that the benefits of the technique can be had without the attendant suffering and the very real risks of adverse effects on psychology and nutrition.[1] This is a promising area of research, and it will be covered here in considerable detail on an ongoing basis. However, this is not the time to start any discussion of specific ‘evidence based’ technologies for extending healthy lifespan. Indeed, before we go any further, it is necessary to become familiar with the concept of evidence based medicine (EBM) (Figure 2).
Evidence Based Medicine
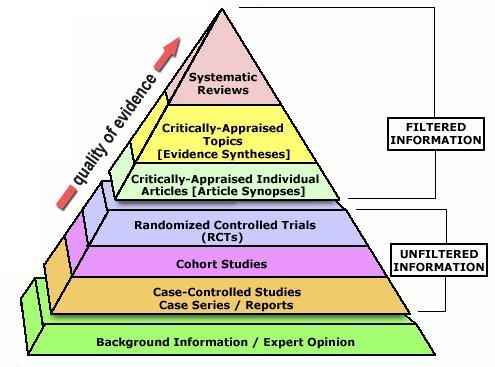
Figure 2: Detailed Diagrammatic representation of the levels of evidence used in Evidence Based Medicine.
Evidence-based medicine (EBM), also called evidence-based practice (EBP) aims to apply the best available evidence gained from the scientific method to clinical decision making. It seeks to assess the strength of evidence of the risks and benefits of treatments, including the lack of treatment, and diagnostic tests.Evidence quality can range from meta-analyses and systematic reviews of double-blind, placebo-controlled clinical trials at the top of the pyramid (above), to conventional wisdom at the bottom.
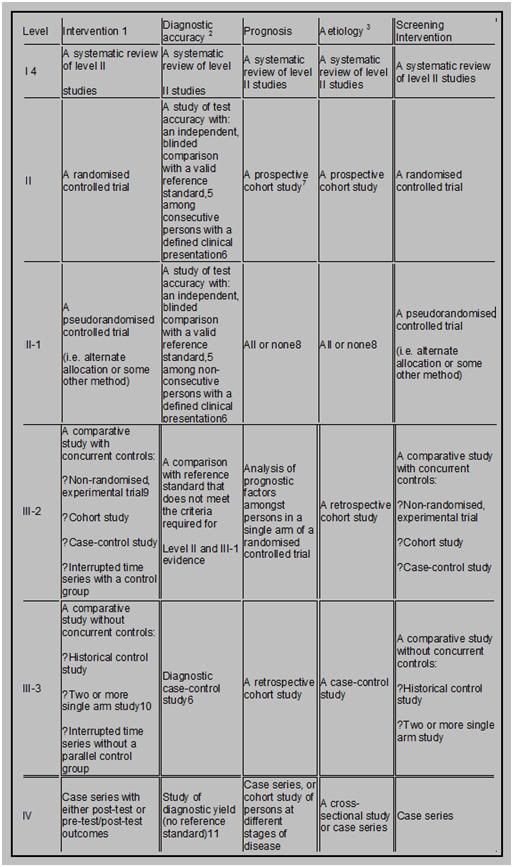
The discrete types or levels of evidence I will be using in all my discussions here on Chronosphere are those of the Centre for Evidence Based Medicine (CEBM), as set out in their “’Levels of Evidence’ Document” which is reproduced, below.
1. A summary of how evidence can be graded.
In simple terms, one way of looking at levels of evidence is as follows (the higher the level, the better the quality; the lower, the greater the bias):
 or…
or…
- Category I: Evidence from at least one properly randomized controlled trial.
- Category II-1: Evidence from well-designed controlled trials without randomization.
- Category II-2: Evidence from well-designed cohort or case-control analytic studies, preferably from more than one center or research group.
- Category II-3: Evidence from multiple times series with or without intervention or dramatic results in uncontrolled experiments such as the results of the introduction of penicillin treatment in the 1940s.
- Category III: Opinions of respected authorities, based on clinical experience, descriptive studies and case reports, or reports of expert committees.
[Source: Harris, R.P. et al. (2001). Current methods of the U.S. Preventive Services Task Force: a review of the process. American Journal of Preventive Medicine. April 20 (3 Supplement): 21-35.]
Not surprisingly, the place to start in looking for any reliable method(s) of life extension is at the top of the evidence pyramid, which consists of Systematic Reviews (including well designed meta-analyses) and Randomized Double Blind Clinical Studies.
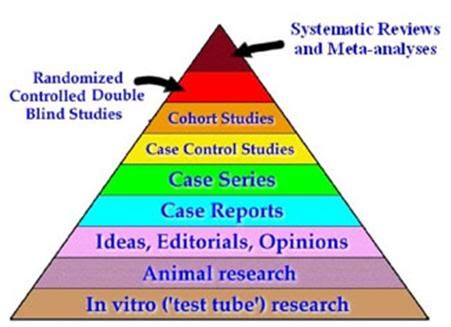 Figure 3: The EBM pyramid made simple.
Figure 3: The EBM pyramid made simple.
The majority of “amateur interventive gerontologists,” or active “life extensionists” who are pursuing lifespan extending therapies on themselves are usually both surprised and dismayed when looking at this pyramid (Figure 3). The first reason for this is that either all, or almost all, of the interventions they are using are at the very bottom of the pyramid. The second reason for the shock and dismay (and often disbelief) is that animal and in in vitro research rank below the ideas, editorializing and opinions of medical professionals, instead of at the top of the pyramid, where most activist life extensionists typically feel they should belong.
However, the fact is that very little animal, or in vitro research has any direct clinical applicability to humans.[2-4] This is not because government regulations or “greedy” pharmaceutical companies don’t want people to benefit from disease-curing or life extending drugs, but rather, because the vast majority of that research is either bad (junk) science or it fails to translate to humans.[4-10] Even when animal studies are well designed and carried out in relevant animal models of disease and show strongly positive results, mostly these findings fail to translate to humans. There are many reasons for this, but chief amongst them is that animals, despite their high ‘percentage’ of genetic overlap with humans, are really biochemically sufficiently different that the findings aren’t applicable to humans. The public are bombarded with numbers, such as chimpanzees are 96% to 98% genetically homologous with humans; cats: 90%, dogs: 82%, cows: 80%, rats: 69% and mice: 67% (http://www.ncbi.nlm.nih.gov/homologene). These numbers get even more impressive when it is noted that 75% of mouse genes have equivalents in humans and 90% of the mouse genome can be matched to a comparable region on the human genome. In fact, recent research indicates that ~ 99% of mouse genes turn out to have analogs in humans.

Figure 4: If we were mice, most cancers would be treatable or cured, there would be effective drugs for stroke and cerebral ischemia, and a wide range of other conditions would have effective therapies. However, we are not mice.
So what’s the problem with the applicability of animal research to humans? Well, consider that at in 3 out of ten patients the drug prescribed for them fails to work. It’s not that the patient is non-compliant or just doesn’t get better; it is that the drug failed to have the anticipated therapeutic effect. Thus, in those patients, the drug was a waste of money and time; and to the extent that it may have adverse effects, a real danger. In fact, there are 2.2 million serious cases of adverse drug reactions (ADRs) and over 100,000 deaths each year in the US. That makes (ADRs) one of the leading causes of hospitalization and death in the US! Most people take ADRs and lack of therapeutic effect in the drugs they are prescribed (or purchase over the counter (OTC)) for granted. “Oh, that doesn’t work for me,” or “I can’t take that because…” are commonplace remarks. And they apply to people who use only “natural” or herbal remedies as much or more as they do those who use “synthetic” drugs.
The reason for these phenomena is very instructive about why animal research turns out to have so little applicability to humans. The cause of the huge variation in responsiveness to drugs in humans is genetic variation between individuals; even identical twins are not genetically identical, due to mutations and to variations in gene activation (epigenetic factors).[11] There are two types of genetic variations known to impact drug metabolism; copy number variation, which results from deletions, inversions, insertions and duplications in genes, and nucleotide variations, or single nucleotide polymorphisms (SNPs). It is estimated that approximately 0.4% of the genomes of unrelated people typically differ with respect to gene copy number. The nucleotide diversity (SNPs) between humans is about 0.1%, which is 1 difference per 1,000 DNA base pairs! Combine these two numbers and human genetic variation is estimated to be at least 0.5% or, if you prefer, 99.5% similarity between individuals.[11-13]
That seemingly trivial amount of genetic variation is responsible for the observed and well documented large disparity in response to therapeutic drugs observed within the human species. Even the SNPs (pronounced “snips”) have a profound effect on the response (or lack thereof) to therapeutic drugs and they are the sources of a major research effort to develop a catalog of SNPs that can be used as a diagnostic tool to predict and individual person’s drug response. This rapidly developing area of research is called pharmacogenomics and it has already seen clinical application in cancer chemotherapy, anticoagulant dosing, the treatment of Hepatitis C and psoriasis, and in seizure disorders.[14-20]
New Drug Development: May I Suggest Roulette, Instead?
A few more words need to be said about the drug development research and success. Leaving animal data aside, most human clinical trials to evaluate refinements of existing (and proven) drugs or therapies either fail, or result in active harm.[2, 21-23] The chances of a novel molecule making it from in vitro or animal testing to clinical use in humans are ~ 1,000 to 1. You’d be much, much better off playing straight-up roulette, where the odds against you are only 37 to 1. Even in studies or clinical trials where there are ample existing theory and prior in vitro, animal research and clinical trials data that were positive and point compellingly to a favorable outcome, trials often fail.
 A good example of this with direct relevance to life extensionists is the saga of vitamin E in the treatment and prevention of atherosclerosis, and in particular, coronary artery disease.There are many animal experiments showing that vitamin E reduces or inhibits the development of atherosclerosis. Epidemiological studies in humans provided robust support to these data, since consumption of vitamin E in the diet was inversely associated with mortality from cardiovascular disease.[24, 25] And to the theoreticians and mechanists, there was the perhaps even more compelling fact that the free radical biochemistry implicated as being a primary factor underlying atherogenesis (oxidized low density lipoprotein (LDL)) is favorably impacted by the addition of vitamin E and similar chain breaking antioxidants to the diet in supraphysiological amounts.[26] The free radical theory of aging also supports the idea that vitamin E and other antioxidant molecules might reduce the incidence of degenerative disease, and perhaps retard aging. Further, in accordance with both theory and the animal data, administration of vitamin E to human volunteers reduced the level of lipid peroxidation, and in particular reduced the level of oxidized LDL.[27]
A good example of this with direct relevance to life extensionists is the saga of vitamin E in the treatment and prevention of atherosclerosis, and in particular, coronary artery disease.There are many animal experiments showing that vitamin E reduces or inhibits the development of atherosclerosis. Epidemiological studies in humans provided robust support to these data, since consumption of vitamin E in the diet was inversely associated with mortality from cardiovascular disease.[24, 25] And to the theoreticians and mechanists, there was the perhaps even more compelling fact that the free radical biochemistry implicated as being a primary factor underlying atherogenesis (oxidized low density lipoprotein (LDL)) is favorably impacted by the addition of vitamin E and similar chain breaking antioxidants to the diet in supraphysiological amounts.[26] The free radical theory of aging also supports the idea that vitamin E and other antioxidant molecules might reduce the incidence of degenerative disease, and perhaps retard aging. Further, in accordance with both theory and the animal data, administration of vitamin E to human volunteers reduced the level of lipid peroxidation, and in particular reduced the level of oxidized LDL.[27]
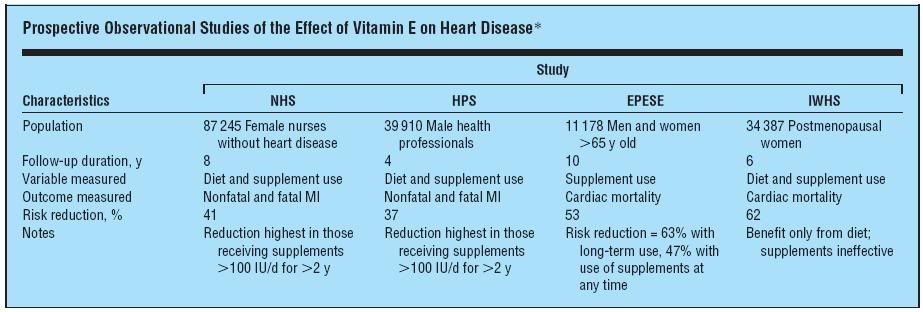 Figure 5:*NHS indicates Nurses’ Health Study; HPS, Health Professionals’ Follow-up Study; EPESE, Established Populations for Epidemiologic Studies of the Elderly; IWHS, Iowa Women’s Health Study; MI, myocardial infarction; and ellipses, none.
Figure 5:*NHS indicates Nurses’ Health Study; HPS, Health Professionals’ Follow-up Study; EPESE, Established Populations for Epidemiologic Studies of the Elderly; IWHS, Iowa Women’s Health Study; MI, myocardial infarction; and ellipses, none.
Several prospective studies in which vitamin E was given as a supplement, including the US Nurses’ Health Study[28] and the US Health Professionals’ Follow-up Study, found a 34% and 39% reduction (respectively), in the incidence of myocardial infarction, [29] More impressively still, the Iowa Women’s Health Study found a 47% reduction in cardiac mortality.[30] These were not small studies published in obscure journals. They were very large trials (Figure 5) and they were published in the New England Journal of Medicine. So what’s the problem? The problem was that other researchers could not duplicate the results and so subsequent, carefully designed trials were conducted.
The largest and best designed of these was the a randomized, placebo-controlled Medical Research Council/British Heart Foundation (MRC/BHF) Heart Protection Study in which antioxidant vitamin supplementation was examined in 20,536 individuals with coronary disease, other occlusive arterial disease, or diabetes mellitus. The study participants were randomized to receive vitamin E (600 mg), vitamin C (250 mg), and beta carotene (20 mg) daily or matching placebo. Intention-to-treat comparisons of outcome were conducted among all participants. An advantage to this study was that critics of earlier failed trials pointed out that vitamin E can act as a pro-oxidant in the absence of vitamin C and that it has in vitro pro-oxidant activity in cell membrane lipids under some conditions. In vivo, vitamin C is the molecule which disposes of the water soluble radical species that can be generated by vitamin E and beta carotene was added to scavenge lipid soluble radicals.
The MRC/BHF study found no significant differences between the vitamin and placebo groups in all-cause mortality, or in deaths caused by vascular or nonvascular conditions. Nor were there any significant differences between groups in the incidence of nonfatal myocardial infarction or sudden cardiac death, nonfatal or fatal stroke, or coronary or non-coronary re-vascularization. In fact, the study found that the use of antioxidant vitamins did not produce any significant reductions in 5-year mortality from, or incidence of, any type of vascular disease, cancer, or other major outcome, compared with placebo.[31]
Other studies also showed no benefit [32-34] and there was even some suggestion of harm in the form of an apparent increase in mortality and morbidity from gastrointestinal and intracranial bleeding. In 2009, a metanalysis of vitamin E supplementation trials by Dotan, et al., using Markov model analysis showed that the vitamin E supplemented “virtual cohort” had 0.30 decrease in their quality-adjusted life year (QALY) (95%CI 0.21 to 0.39) compared to the non-treated “virtual cohort.”[35] QALY is a statistical measurement tool used to evaluate not just death or discrete injurious events, such as heart attack or hemorrhagic stroke, but rather measure these events, along with all deaths or debilities as a single entity, and report them in terms of how much loss or gain of functional life occurs in a given group. This work supports an earlier metanalysis showing increased all-cause mortality associated with vitamin E doses ~500 mg/day or more. When a metanalysis was done to look specifically for the effects of vitamin E on stroke it was found that vitamin E increased the risk for hemorrhagic stroke by 22% and reduced the risk of ischemic stroke by 10%.[1]
The metanalysis indicating that vitamin E supplementation (≥500 mg q.d.) is associated with an increase in morbidity and mortality is consistent with the known effect of vitamin E in such doses on bleeding time. Supraphysiologic vitamin E antagonizes vitamin K and causes platelet dysfunction resulting in an increased prothrombin time. It is almost axiomatic in medicine that any increase in bleeding time (anticoagulation) is associated with an increased incidence of clinically significant gastrointestinal (GI) and intracranial bleeding. For vitamin E to show benefit, it would be necessary for any increase in adverse effects to be offset by the benefits it conferred. For vitamin E, this was not the case, whereas for aspirin, which also increases bleeding time and causes an increased incidence of GI and intracranial bleeding, shows such strong benefit in the reduction of myocardial infarction that it is worth the associated risk in the appropriate patient population (i.e., those 50 or over and those with known cardiovascular disease).
This kind of “reversal of fortune” happens over and over again in medicine with respect to drugs as as to other treatment interventions and it is one of the well justified reasons why the astute clinician is very skeptical about putative therapies to treat disease that have not been scientifically vetted – preferably repeatedly, internationally and in well designed and executed trials. It is thus an unfortunate reality that no matter how compelling a therapy seems theoretically or in the laboratory, it still must be proven clinically. And it is even truer that the overwhelming majority of putative therapeutic interventions either fail to work, or injure or kill the patient. There is absolutely no reason to think that this will not be the case with putative life extension drugs.
 It is also usually the case that taking multiple drugs, or polypharmacy as it is formally known, negatively shifts the risk to benefit ratio (especially in the ill the debilitated or the elderly). This is so because the biochemistry of living systems is not only enormously complex; it is also interdependent and self regulating. The vast majority of drugs, or supraphysiological doses of nutrients, will perturb multiple biochemical pathways and the more molecules administered, the more likely it becomes resulting adverse interactions will occur. It is, as the Taoist maxim cautions, virtually impossible “to do just one thing” when dealing with a complex and dynamic system. Alter one part of the system in a desirable way and there will likely be consequences in other parts of it – and the odds are high that they will not be favorable.[2]
It is also usually the case that taking multiple drugs, or polypharmacy as it is formally known, negatively shifts the risk to benefit ratio (especially in the ill the debilitated or the elderly). This is so because the biochemistry of living systems is not only enormously complex; it is also interdependent and self regulating. The vast majority of drugs, or supraphysiological doses of nutrients, will perturb multiple biochemical pathways and the more molecules administered, the more likely it becomes resulting adverse interactions will occur. It is, as the Taoist maxim cautions, virtually impossible “to do just one thing” when dealing with a complex and dynamic system. Alter one part of the system in a desirable way and there will likely be consequences in other parts of it – and the odds are high that they will not be favorable.[2]
Thus, in making decisions about which putative life extension therapies to use, the most rational course is to start with those where there is Level-1 evidence of benefit. That may not even seem possible, since there are no known lifespan extending drugs or treatments in humans, let alone ones that have undergone extensive, well designed and repeated clinical trials. Or are there? The answer to that question will be the subject of the next article in this series.
Footnotes
[1] While the 10% reduction in the risk of ischemic stroke may seem promising this is really constitutes no advantage since hemorrhagic strokes have a far higher mortality and morbidity rate than is the case for ischemic stroke.
[2] Like mutations, most arbitrary alterations to the biochemistry or gene expression of a complex living system are not likely to result in benefit.
References
1. Ingram D, Zhu, M, Mamczarz, J, Zou, S, Lane, MA, Roth, GS, deCabo, R.: Calorie restriction mimetics: an emerging research field. Aging Cell 2006, 5(2):97-108.
2. Ikonomidou C, Turski L: Why did NMDA receptor antagonists fail clinical trials for stroke and traumatic brain injury? Lancet Neurol 2002, 1(6):383-386.
3. Ozdemir FN, Akcay A, Elsurer R, Sezer S, Arat Z, Haberal M: Interdialytic weight gain is less with the Mediterranean type of diet in hemodialysis patients. J Ren Nutr 2005, 15(4):371-376.
4. Whiteside GT, Adedoyin A, Leventhal L: Predictive validity of animal pain models? A comparison of the pharmacokinetic-pharmacodynamic relationship for pain drugs in rats and humans. Neuropharmacology 2008, 54(5):767-775.
5. Harber LC, Armstrong RB, Ichikawa H: Current status of predictive animal models for drug photoallergy and their correlation with drug photoallergy in humans. J Natl Cancer Inst 1982, 69(1):237-244.
6. Olson H, Betton G, Robinson D, Thomas K, Monro A, Kolaja G, Lilly P, Sanders J, Sipes G, Bracken W et al: Concordance of the toxicity of pharmaceuticals in humans and in animals. Regul Toxicol Pharmacol 2000, 32(1):56-67.
7. Pound P, Ebrahim, S, Sandercock, P, Bracken, MB, et al.: Where is the evidence that animal research benefits humans?: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC351856/pdf/bmj32800514.pdf. BMJ 2004, 328:514-517.
8. Dixit R, Boelsterli UA: Healthy animals and animal models of human disease(s) in safety assessment of human pharmaceuticals, including therapeutic antibodies. Drug Discov Today 2007, 12(7-8):336-342.
9. Caldwell J: Problems and opportunities in toxicity testing arising from species differences in xenobiotic metabolism. Toxicol Lett 1992, 64-65 Spec No:651-659.
10. Wilbourn J, Haroun L, Heseltine E, Kaldor J, Partensky C, Vainio H: Response of experimental animals to human carcinogens: an analysis based upon the IARC Monographs programme. Carcinogenesis 1986, 7(11):1853-1863.
11. Bruder CE, Piotrowski A, Gijsbers AA, Andersson R, Erickson S, Diaz de Stahl T, Menzel U, Sandgren J, von Tell D, Poplawski A et al: Phenotypically concordant and discordant monozygotic twins display different DNA copy-number-variation profiles. Am J Hum Genet 2008, 82(3):763-771.
12. Sachidanandam R, Weissman D, Schmidt SC, Kakol JM, Stein LD, Marth G, Sherry S, Mullikin JC, Mortimore BJ, Willey DL et al: A map of human genome sequence variation containing 1.42 million single nucleotide polymorphisms. Nature 2001, 409(6822):928-933.
13. Cargill M, Altshuler D, Ireland J, Sklar P, Ardlie K, Patil N, Shaw N, Lane CR, Lim EP, Kalyanaraman N et al: Characterization of single-nucleotide polymorphisms in coding regions of human genes. Nat Genet 1999, 22(3):231-238.
14. Beaulieu M, de Denus S, Lachaine J: Systematic review of pharmacoeconomic studies of pharmacogenomic tests. Pharmacogenomics, 11(11):1573-1590.
15. Beery TA, Smith CR: Genetics/genomics advances to influence care for patients with chronic disease. Rehabil Nurs, 36(2):54-59, 88.
16. Cacabelos R, Hashimoto R, Takeda M: Pharmacogenomics of antipsychotics efficacy for schizophrenia. Psychiatry Clin Neurosci, 65(1):3-19.
17. Johnson JA, Liggett SB: Cardiovascular pharmacogenomics of adrenergic receptor signaling: clinical implications and future directions. Clin Pharmacol Ther, 89(3):366-378.
18. Schwab M, Schaeffeler E, Zanger UM, Brauch H, Kroemer HK: [Pharmacogenomics: hype or hope?]. Dtsch Med Wochenschr, 136(10):461-467.
19. Kamal SM: Hepatitis C virus genotype 4 therapy: progress and challenges. Liver Int, 31 Suppl 1:45-52.
20. Yoshida S, Sugawara T, Nishio T, Kaneko S: [Personalized medicine for epilepsy based on the pharmacogenomic testing]. Brain Nerve, 63(4):295-299.
21. Wiendl H, Neuhaus O, Kappos L, Hohlfeld R: [Multiple sclerosis. Current review of failed and discontinued clinical trials of drug treatment]. Nervenarzt 2000, 71(8):597-610.
22. Corman LC, Davidson RA: Why clinical trials fail: the hidden assumptions of clinical trials. South Med J 1992, 85(2):117-118.
23. Krum H, Tonkin A: Why do phase III trials of promising heart failure drugs often fail? The contribution of “regression to the truth”. J Card Fail 2003, 9(5):364-367.
24. Rimm E, Stampler, MJ, Ascherio, A, Giovannuci, E, Willett, GA, Colditz, WC.: Vitamin E consumption and the risk of coronary heart disease in men. N Engl J Med 1993, 328::1450-1455.
25. Stampfer M, Hennekens, CH, Manson, JE, Colditz, GA, Rosner, B, Willett, WC.: Vitamin E consumption and the risk of coronary disease in women. N Engl J Med 1993, 328:1444-1449.
26. Stampfer M, Rimm, EB: Epidemiologic evidence for vitamin E in prevention of cardiovascular disease. Am J Clin Nutr 1995, 62:1365S-1369S.
27. Reaven P, Witztum JL.: Comparison of supplementation of RRR-alpha-tocopherol and racemic alpha- tocopherol in humans. Effects on lipid levels and lipoprotein susceptibility to oxidation. Arteriosclerosis, Thrombosis, and Vascular Biology 1993, 13:601-608.
28. Stampfer M, Hennekens, CH, Manson, JE, Colditz, GA, Rosner, B, Willett, WC.: A prospective study of vitamin E consumption and risk of coronary disease in women. N Engl J Med 1993, 328:1444-1449.
29. Rimm E, Stampfer, MJ, Ascherio, A, Giovannucci, E, Colditz, GA, Willett, WC.: Vitamin E supplementation and the risk of coronary heart disease among men. N Engl J Med 1993, 328:1450-1456.
30. Kushi L, Folsom, AR, Prineas, RJ, Mink, PJ,Wu,Y, Bostick, RM.: Dietary antioxidant vitamins and death from coronary heart disease in postmenopausal women. N Engl J Med 1996, 334:1156-1162.
31. Aizawa K, Shoemaker JK, Overend TJ, Petrella RJ: Metabolic syndrome, endothelial function and lifestyle modification. Diab Vasc Dis Res 2009, 6(3):181-189.
32. Yusuf S, Dagenais, G, Pogue, J, Bosch, J, Sleight, P.: Vitamin E supplementation and cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study Investigators: http://content.nejm.org/cgi/content/full/342/3/154. N Engl J Med 2000;, 342(3):154-160.
33. Lonn E, Bosch, J, Yusuf, S, Sheridan, P, Pogue, J, Arnold, JM, et al.: HOPE and HOPE-TOO Trial Investigators. Effects of long-term vitamin E supplementation on cardiovascular events and cancer: a randomized controlled trial. JAMA 2005;, 293(11):1338 -1347.
34. Vivekananthan D, Penn, MS, Sapp, SK, Hsu, A, Topol, EJ.: Use of antioxidant vitamins for the prevention of cardiovascular disease: meta-analysis of randomized trials. Lancet 2003, 1:2017 -2023.
35. Dotan YP, I. Lichtenberg, D. Leshno, M.: Decision analysis Supports the paradigm that Indiscriminate supplementation of vitamin E does more harm than good. Arterioscler Thromb Vasc Biol 2009, 29:1304-1309.

FWIW, I don’t think it’s a Taoist maxim (not one I’ve read before), but a version of Garrett Hardin’s ‘First Law of Ecology’: “You cannot do only one thing.”
Dunno, I’ve been using that quote since the late 1970s. I think I read it in a book of quotations with accompanying commentary, because I remember reading the quote and thinking, “that’s a really idiotic quote.” The subsequent explanation enlightened me that what was meant is that everything in the universe is interconnected and you can’t act on one part without affecting the whole. I was still unimpressed with the quote until I started to understand trying to intervene in complex systems in only one way – be they biological or social. THEN the wisdom of the quote became apparent. — Mike Darwin
Good economic thinking emphasizes that principle as well. We see the principle in action when a top-down government intervention into the economy intended to “fix” a problem usually generates new and unanticipated problems.
Speaking of polypharmacy, what do you make of the Polycap clinical trial in India?
Great idea. It’s already being done here in the form of combo pills for BP. — MD
Have you taken on TA-65 as the next “miracle pill” and I just missed it? It has only been tested seriously for a few years (under the FDA radar as a supplement extracted from astragalus). The first three years with the price barrier being so high they had about 100 whom they followed closely with monitoring -in case repairing telomeres -increasing/activating telomerase causes cancer. The last (4th year) the price having come down so more can afford it, but now many are on that are not carefully monitored.
I’ve wondered if it will come out as the next Vitamin E or some such failure. That said, to be on-topic about Calorie Restriction -I’ve been doing it for 10 years. My intention for starting and following it was more for extending my healthy middle age years–which I think I’m in now at 36 ;) -regardless, the extra years it may give at the end of life are pretty insignificant if you go with a 3% increase as some speculate it would give in regards to human. I personally though, care more about my middle ages-since I love being alive and healthy. I having been active daily, and often a few times a day for decades in my love life, I never find that boring–in fact never did in my first ten year marriage or in now in the fifth year of my current marriage. I know others who still are in love, and things are never boring–an excellent thing for physical and mental health. As a woman, I feel CR has helped me in that area, but I do exercise a moderate amount as well. Ones mental health is important if one is to raise children, and give back to their community through work or volunteering.
Unlike some, I do not fear old age, and just today had to find a distinguished looking model for my husband’s company’s website. We needed white hair so I enlisted a friend from my UU church. I look forward to the added wisdom of old age, and respect it gives. I also intend to be as healthy as possible, and at least know that cuddling hormones are still beneficial in advanced age if my husband and I don’t have the energy that we have now. I figure that if I’m happy I can give back more to my community, but giving back makes me happy as well as my home life. Of course in my old age I also have being a grand parent to look forward too–I’ve promised my kids I’ll even re-lactate to help raise grand children if any of them can not breastfeed due to their careers. (in case you are wondering, back when wet-nurses were common, one of the oldest licensed wet-nurses on record was 76, she could only take on 2 babies at that time instead of 4 like when she was younger–also in many cultures grandmas would care for and re-lactate for their grandchildren). I have a lot of things to look forward to in my advanced age :)
I support extreme life extension in a myriad of areas though, because I love living–but as I’ve pointed out before, I also try to give back to my community and think we have a long ways to go to bring the standards of living up around the world to more equitable allocations of wealth, medical care, education and opportunities.
Basically though think more would have increased energy in their middle ages if they implemented Calorie Restriction, and that if we have any actual regenerative drugs come along then the more the better.
As it was originally marketed, with full disclosure about the risk of cancer and the unknown risk of other adverse effects, I didn’t have any problem with TA-65, The high price tag was also a plus, because that pretty much rules out the clueless and foolish who’ll shell out $29.995 for anything a persuasive infomercial says will work. If the drug really does extend lifespan dramatically, but also causes cancer, that might be manageable with enough money for sophisticated early diagnosis and increasing better targeted molecular and immune-cell engineered Txs for cancer coming on line.
In fact, this pretty much the way any meaningful drug research will get done in humans, and it is how it gets done now. For instance, take Vioxx. Poor Merk! Vioxx probably causes no more heart attacks than ibuprofen and it certainly didn’t kill as many people as aspirin does each year in the US. Consider that there were 7,600 deaths and 76,000 hospitalizations in the US last year due to NSAIDS (NSAIDs include aspirin, ibuprofen, naproxen, diclofenac, ketoprofen, and tiaprofenic acid.)! You have to be pretty sick to be hospitalized. The Phase I – III clinical trial size is simply too small to show that a drug causes 1 in 1,000, let alone 1 in 5,00o or 1 in 10,000 people to drop over dead and to do so with no prior toxicity, or signs of toxicity (abnormal labs, etc.). There is a drug that it a godsend to many patients with multiple sclerosis called TYSABRI (natalizumab). Unfortunately, it greatly increases the risk of progressive multifocal leukoencephalopathy (PML), an opportunistic viral infection of the brain that usually leads to death or severe disability. The FDA wanted to pull it. The incidence of PML is much higher than would normally be considered acceptable as an adverse effect in a drug, and MS is mostly a slow killer. PML didn’t show up on any of the clinical trials because they were not powered adequately for such an “infrequent but too frequent” adverse effect. And so it was for Vioxx, and so it will be for almost all drugs where the incidence of adverse reactions is so low that tens of thousands or hundreds of thousands of people would have to be in the clinical trials. As it is, ~ 1/3rd to 1/2 of all new drugs are pulled from the market after 3 years, because of adverse effects. And if the adverse effect is something like a heart attack or stroke that lots of people taking the drug might suffer, even if they didn’t take it, it becomes a very, very costly proposition to sort it out. Animal testing is almost useless for determining drug safety and efficacy in humans – although it works outstandingly for the animal species being tested. — Mike Darwin
I have no interest in TA-65 because I don’t think telomere shortening is a cause of aging. The differential turn over rates of different cell types in the body make clear that telomere maintenance is a regulated process. Whatever the real cause of aging (I’m convinced its mitochondrial dysfunction), it damages telomere maintenance just as it damages everything else. This is why I think TA-65 is unlikely to work as a life extension agent. Mitochondrial biogenesis is necessary for life extension.
Vioxx inhibits vascular growth, which is why it is associated with heart attacks and strokes. Since cancer cells rely on greater vascularization than regular cells, this suggests that Vioxx was used for the wrong purpose. It seems to me the Vioxx would be useful as part of a regiment to treat cancer.
I think the jury is still out on telomeres in aging in humans. I’ll be discussing that in due time, so I won’t go into it here. While mitochondrial decay, and thus possibly mitochondrial biogenesis, seem a promising approach to extending lifespan, it simply isn’t credible that the mitochondria are the primary motors of aging. Aging is a multi-system failure of maintenance and regeneration from the subcellular to to the tissue and organ levels. Again, I won’t go there now, because I’m going there later in a more rigorous and detailed way.
As to Vioxx, it is probably a little better or worse than a number of the non-selective COX-I / COX-II inhibitors still on the market. The difference is that the others were old drugs that a lot of people like and need. And they are still in use today and readily available OTC. No one has done the kind of rigorous study of the CVD morality and morbidity from these OTC drugs that was done for Vioxx, because it would be problematic (they are in universal use) and incredibly costly. As to cancer Tx, there are much better angiogenesis inhibitors than Vioxx.
My point was that other NSAID drugs wreak more death and mayhem than Vioxx did every year, and yet thy are sold OTC and no one gives the truly incredibly morbidity and mortality a second thought. Any GP or ED doc will regurgitate countless stories of serious GI bleeding due to NSAIDS (and especially aspirin) on cue. Of course, they don’t mention all the hemorrhagic strokes caused by aspirin’s anti-platelet activity because they have no way to distinguish those from “regular strokes” and with so much of the population on aspirin that wouldn’t be easy.
Aspirin causes a truly gruesome and often fatal condition in children called Reye’s syndrome, and if it were any other drug than aspirin, it WOULD have been pulled from the market, Instead, a massive educational campaign was launched to teach parents not to give sick children aspirin – the rational thing to do! However, meanwhile (until the population was educated), children continued to be neurologically maimed and killed by Reye’s. I’ve dialyzed youngsters with multi-system organ failure from Reye’s and it is a wretched and heartbreaking illness with a poor outcome.
Beyond the COX-inhibiting NSAIDS, there is “Tylenol,” or more properly, acetaminophen (APAP) (paracetamol in the rest of the world). Johnson&Johnson/MacNeil are apparently getting tired of paying for liver transplants and paying out judgments for people who die of liver failure because this hepatotoxic drug has spread into almost every product on the market for pain or discomfort, ranging from nostrums for menstrual cramps to sleep aids. APAP toxicity is the most common cause of hepatic failure requiring liver transplantation in Great Britain. In the United States, APAP toxicity has replaced viral hepatitis as the most common cause of acute liver failure, and it is the second most common cause of liver failure requiring transplantation in the US.The percentage of cases of acute liver failure caused by an overdose of acetaminophen increased considerably from 1998 to 2003, with unintentional overdose accounting for at least half of these case. Acetaminophen (APAP) is now the drug of choice for suicide in the US & UK and the number of deaths and hospitalizations from APAP has risen steadily since its widespread introduction in the 1960s (it was initially introduced inthe1950s). I can’t find the numbers for the US, but in England and Whales there are ~700 successful suicides/yr using APAP. The drug interacts unpredictably with alcohol in many individuals to cause serious liver toxicity and the economic costs of APAP toxicity are estimated to be in the hundred of millions of dollars/yr. I note that few,if any other PRESCRIPTION, let alone OTC drug, with a decades long history of steadily escalating injury and death to the population. By contrast, Vioxx was a dream drug! So it is the hypocrisy and unfairness of the treatment of Vioxx that I find objectionable.
Having said that, Vioxx was over-prescribed and Merk knew it had a problem long before they acted. Due to biochemical variations in individuals, a given NSAID, like other drugs, may provide great relief to a sub-population of patients, whilst doing nothing, or being no better than existing drugs, for others. It’s use should have been confined to those who really demonstrated substantial benefit, for whom other drugs were ineffective and who were informed of, and accepted the risk. The same is likely true of many other drugs that fare logged relentlessly to a wide populations of patients, such as Crestor and Zyprexa. There are no demon drugs, there are just misused drugs, and some are much easier to misuse than others. Unfortunately, the Pharms have little economic choice but to try to maximize sales for each and every approved drug. At a cost of near a billion per drug approved, it is simply not economical to restrict the use of any approved drug to the population that will benefit most. To recover the enormous capital cost of introducing a new drug it is necessary to sell every milligram of the molecule possible, whether it is the best drug for a given patient, or not.. — Mike Darwin
Quite the contrary, I’m nearly convinced that mitochondria is THE root cause of aging. Nick Lane, among others, has convinced me of this.
I don’t want to let this statement stand un-rebutted – or more accurately, uncorrected. I’m rarely as absolutist as I’m going to be here, nevertheless I will say that there is virtually no chance that mitochondrial dysfunction is THE cause of aging; and I’m surprised that, at this late date, anyone would assert such a “simple” mono-causal theory as the primary cause of aging.
To believe in the mitochondrial theory of aging as the motor of aging is akin to believing that automobiles wear out and fail because of the effects of friction. If only we could find an additive to reduce or eliminate friction, cars wouldn’t age. Friction induced wear is indeed a major cause of failure in the drive train of otherwise well maintained “working” automobiles, and arguably the majority of cars that wear out do so because of friction-related damage. However, if it were possible to eliminate friction, or to replace all the elements of the drive train as they experienced wear and failure, automobiles would still not be immortal – nor would they be spectacularly long lived. Anyone who has kept an old car running well beyond its mean lifespan will immediately understand what I’m getting at here.
The fact is, lots of things can and will go wrong, even in a comparatively simple device like a car and over relatively short periods of time. Hoses and belts will decompose and fail, the windshield and headlamp covers will become pitted and cracked, the upholstery, dashboard and other fittings will oxidize, work harden and fail, the radiator will corrode, the wiring will work harden and break… To put it simply, automobiles were not engineered to run forever. And hardly anyone would seriously suggest that any device or instrumentality would just “continue to run forever” without enormous and very costly effort and engineering. Evolution is not immune from these constraints, and in fact is arguably more driven by them than are human engineering efforts. Life didn’t arise as a perfectly working system of immortal organisms. Such immortality as exists in the biological world exists only in the form of reproduction. Reproduction is exactly the elaborately complex and cunningly engineered system we’d expect to find in any system attempting infinite survival.
Individuals are tools used by reproduction to preserve a reasonable facsimile of the genome over very long periods of time. For some organisms, such as ants, termites and many plants, the fidelity and stability of genome preservation is staggering; it is likely that some such organisms from the Permian or the Jurassic could successfully mate with their contemporary counterparts. But mostly, the pressures of the environment transmute the genome, and the organisms that carry it, in remarkable ways. If there has been effective selection pressure for the immortality of complex, multicellular individual organisms, there is no evidence of it.
Any astute observer of human (or mammalian) aging will realize at once that there is simply no engineering and no programming for us to live indefinitely. Many structures, including (importantly) the brain have no provision for indefinite maintenance. Practically from birth on, the brain experiences surprisingly steady and inexorable cell loss. If every neuronal mitochondrion could be kept at peak performance indefinitely (the equivalent of eliminating friction in an automobile), brain cells would continue to fail and die. The damage to neurons as a function of metabolism over time extends to components well beyond the mitochondria. Nuclear DNA damage would eventually prove fatal because there is essentially no nuclear DNA repair in either neurons or glial cells. There are many, many other examples of “absent maintenance” algorithms in complex multicellular organisms.
The good news is that if we look around in the natural world we can find in other organisms (and even in our own genome) many of the maintenance algorithms we’ll need if we are to become practically immortal. But what we will not find is the meta-level organization and implementation of these essential bits and pieces into a coherent, working system that will allow for the indefinite operation of dogs or cats or people. Aging isn’t some “bad mojo” that happened to a previously immortal system, anymore than an automobile wearing out is due to some deficiency in the fuel, the lubricants, or to the mechanic’s carelessness. It is possible not only to to keep an automobile running indefinitely, but to keep it in tip top condition. The British cryonicist Alan Sinclair is a master at this – in fact, he can restore devastated autos to pristine condition. However, in order to do this he has had to apply an enormous body of knowledge and clever techniques (many of which he has invented himself) which were completely outside of the manufacturer’s original design, or of their anticipation of the longevity of their product. Indeed, having watched Alan restore a number of vintage cars it easy to see that a lot of his hard labor, physical and intellectual, is due to the very fact that the manufacturers did not engineer the system for full maintenance.
Engineering biological immortality is going to be a hard, long business. It’s a common human failing that we expect that things we build (and do not understand well) will simply go on forever. This is not the case. To achieve that end requires enormous engineering and effort. — Mike Darwin
This has been written here:
“To believe in the mitochondrial theory of aging as the motor of aging is akin to believing that automobiles wear out and fail because of the effects of friction. If only we could find an additive to reduce or eliminate friction, cars wouldn’t age. ”
Friction also keeps the car alive or in a functional state. Bolts, nuts and screws are used as fasteners within cars. And to keep these items fastened friction is necessary. (I won’t complicate matters here by mentioning that a nut can be welded to a bolt etc)
If a lubricant is added to the thread of a bolt and a nut, the following results: The coefficient of friction is reduced significantly. For the fastener (nut bolt combination) to maintain the same torque value, it is necessary to increase the tightening, which may damage the threads or stretch the fastener beyond its elastic limit, thereby reducing its ability to clamp.
By way of example and as you obviously know, within a car/car engine, the cylinder head conventionally is bolted to the cylinder block, the crankshaft main bearings assembly is bolted to the crankcase etc.
There was a Mechanical Engineering Professor, who I once knew, whose main focus was on friction. He use to say that the whole world is kept together by friction.
Therefore, friction in many ways is good, but yes in some cases it can be bad.
Delusion is incredibly prevalent, and easy to fall into. It seems the older I get the more I realize this. (Granted, it is probably not age so much as education that drives this home.) But plenty of things go beyond mere self-delusion and into a realm where deliberate deception of others is (almost!) certainly the aim. Take the claims of Dr. Joel Wallach, which were some of the first life extension claims I ever heard as a kid. They were passed around in audio tape form as part of an MLM scheme, and lots of people (myself included, it shames me to say) took them for gospel. Here’s a good debunking of the claims from an actual nutritionist: http://nutra-smart.net/al.htm
I sometimes sort of fantasize that the kind of charismatic spiel used so effectively by Wallach and others could be employed for a positive purpose. But is that even possible, without crossing the line ethically, or into the realm of self delusion?
“I sometimes sort of fantasize that the kind of charismatic spiel used so effectively by Wallach and others could be employed for a positive purpose. But is that even possible, without crossing the line ethically, or into the realm of self delusion?”
It is, and you see it every day. It called good PR and advertising. It’s just taken for granted because its so commonplace and because it usually isn’t used to promote frankly fraudulent products. I have a personal loathing for MLM for many reasons. So, it is not easy for me to acknowledge there are MLM operations that are honest, offer reasonable value for money and adequately and fairly compensate those selling the products. Mary Kay and Avon Cosmetics are two examples. AmWay, not so much, IMHO, but they do sell products that are of quality and the sales people do profit. Every time you see an add with mutilated animals asking for money, or are visited by two fresh faced Mormons, you are looking at the same thing.
I remember the colloidal mineral craze Luke ;) I’ve often wished for a charismatic leader in Cryonics–but alas, charismatic leaders often achieve their charm by offering “facts that will extend your life” -some actual ones, but many that are easily falsified. The problem with human life-span is that it takes so many years to prove anything touted as anti-aging or rejuvenating as right or wrong. With Cryonics, we don’t even have a fully functioning mammal that has been preserved for any significant length of time–just evidence of what looks like functional neurons, and other things that show it might work some day. Couple the lack of hard proof with the problems inherent throughout time with human interactions within society and you get what looks like a very poor bet. One that few are willing to take.
Calorie Restriction isn’t even “proven” conclusively, yet more evidence points to it working and there are only a few thousand world wide who actively follow it, hardly more than are signed up for Cryonics.
Just wanted to let you know that there is a study (or more) out there that seems to show that merely having low body fat confers the same longevity benefits of a caloric restriction diet.
Also, there is the Intermittent Fasting diet which is based on multiple studies showing hormonal longevity boosting benefits from fasting.
James, if you have cites on these studies I’d be very grateful if you could post them here. I’d be even more inclined to believe these studies if they pointed to visceral (abdominal) adiposity as a risk. For instance, in both women and men fat in the buttocks, hips and thighs does not show the correlation with CVD or Type II diabetes that visceral fat does, and in fact it may be protective. Visceral fat secretes a range of pro-inflammatory cytokines which damage everything from the vascular endothelium to the beta islet cells in the pancreas. In fact, by the time a person demonstrates an abnormal blood glucose response after a meal (postprandial blood glucose) they are estimated to have already lost 50% to 75% of their beta islet cells. Beta islet cells are non-dividing. By the the time Type II diabetes is clinically apparent, the loss of beta islet cells is estimated to be in the range 0f 75% to 85%. Loss of visceral fat, coupled with exercise, can “reverse” the clinical signs of Type II diabetes by increasing insulin sensitivity and improving the function of the remaining islet cells. However, it does not reverse the underlying loss of beta islet cells. This is one reason that I take exception to the claims of Kurzweil and others that weight loss, diet and exercise can “cure” Type II diabetes. The sad fact is that as many of these people age and experience islet cell loss from “normal” aging, they will once again become diabetic. Indeed, a sub-population of people who develop Type II diabetes do so in the 60s, 70s, 80s, and 90s, despite the absence of any major risk factors. Loss of visceral fat and increase of muscle mass can reverse symptomatic Type II diabetes. That is great, but it doesn’t equate to a cure and the loss of reserve beta islets is likely to translate into increased morbidity and mortality. — Mike Darwin