 By Mike Darwin
By Mike Darwin
First, Try to Make it to the Mean
For the past two months I’ve been asking people I encounter in public places[1] the question, “How old do you think you’ll live to be?” The answer I get from non-smokers is usually a number somewhere between 75 and 90, regardless of their age. Occasionally, people will remark that they expect to live to be100, or even 120 because of “medical advances,” but mostly people put their prospects at or above the mean lifespan for people living in the US. This shouldn’t be surprising, because the mean life expectancy in the US for men and women combined is currently 77.8 years. Since nobody (except for smokers) wants to be less than average, the lowest number people volunteer is right around the mean lifespan for the population of the US, at present.
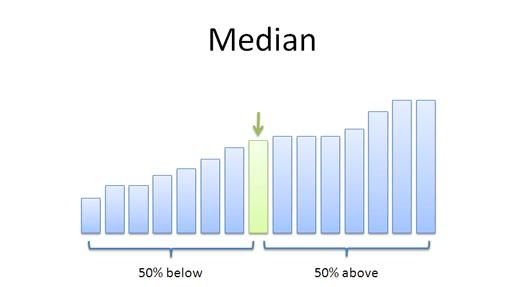 Figure 1: In statistics, a median is described as the numerical value separating the higher half of a sample, a population, or a probability distribution from the lower half. The median of a finite list of numbers can be found by arranging all the observations from lowest value to highest value and picking the middle one. If there are an even number of observations, then there is no single middle value; the median is then usually defined to be the mean of the two middle values. At most, half the population has values less than the median, and, at most, half have values greater than the median. If both groups contain less than half the population, then some of the population is exactly equal to the median. For example, if a < b < c, then the median of the list {a, b, c} is b, and, if a < b < c < d, then the median of the list {a, b, c, d} is the mean of b and c; i.e., it is (b + c)/2.
Figure 1: In statistics, a median is described as the numerical value separating the higher half of a sample, a population, or a probability distribution from the lower half. The median of a finite list of numbers can be found by arranging all the observations from lowest value to highest value and picking the middle one. If there are an even number of observations, then there is no single middle value; the median is then usually defined to be the mean of the two middle values. At most, half the population has values less than the median, and, at most, half have values greater than the median. If both groups contain less than half the population, then some of the population is exactly equal to the median. For example, if a < b < c, then the median of the list {a, b, c} is b, and, if a < b < c < d, then the median of the list {a, b, c, d} is the mean of b and c; i.e., it is (b + c)/2.
However, life expectancy is not the same as mean, or average lifespan. Rather, life expectancy constitutes the expected number of years, on average, that a particular cohort of individuals in the population will survive if the rate of mortality remains constant (until the maximum lifespan is reached).[2] Life expectancy is thus the median number of years, at birth, that a population born in a particular year is expected to survive. For instance, based on the most recent data, life expectancy at birth in 2008 was 77.8 years.[1] The good news for people in this cohort is that half of them will live longer than 77.8 years, and the bad news is that half of them will not survive to their 77th birthday.
Table 1. U.S. Life Expectancy at Birth,
by Sex, in Selected Years
(in years)
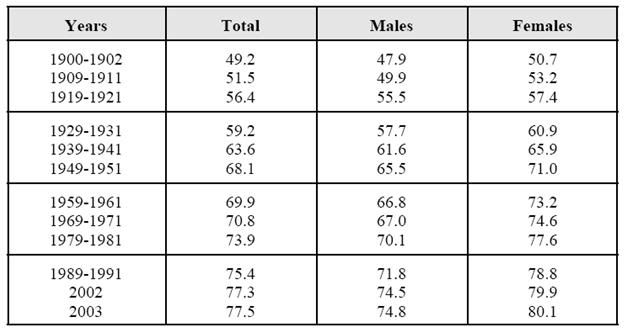 Source: For data through 2002, the Congressional Research Service (CRS) compilation from National Center for Health Statistics (NCHS), United States Life Tables, 2002, National Vital Statistics Reports, vol. 53, no. 6, Nov. 10, 2004. For 2003, NCHS, Deaths: Final Data for 2003, National Vital Statistics Reports, vol. 54, no. 13, Apr. 19, 2006.[3]
Source: For data through 2002, the Congressional Research Service (CRS) compilation from National Center for Health Statistics (NCHS), United States Life Tables, 2002, National Vital Statistics Reports, vol. 53, no. 6, Nov. 10, 2004. For 2003, NCHS, Deaths: Final Data for 2003, National Vital Statistics Reports, vol. 54, no. 13, Apr. 19, 2006.[3]
It is also the case that the lifespan of all of the individuals in the nation does not necessarily increase along with the reported statistical mean lifespan for the nation’s population as a whole. As an example, I was born in 1955, and if we look at the cohort survival data from that period, the median life expectancy for males from my cohort is ~ 66 years. Of course, this includes all males in my cohort, including those who died at birth, those who died in various wars, those who died as a result of youthful indiscretion (some fraction of deaths by accident, suicide and homicide), and those who died due to “random” accidents. A more precise estimate of my life expectancy (and yours) can be had by consulting the chart in Figure 2, below.
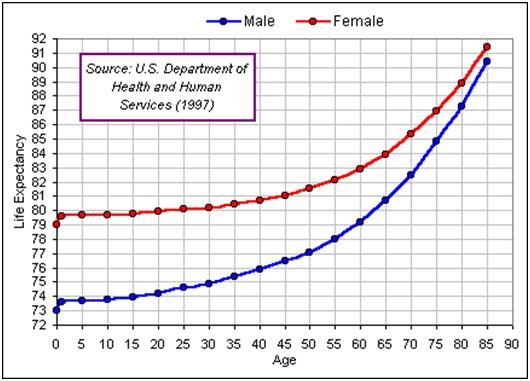 Figure 2: US life expectancy as a function of age (2008 data set).
Figure 2: US life expectancy as a function of age (2008 data set).
Most people seem to assume that they are guaranteed survival to whatever the current mean US lifespan is. Unfortunately, that isn’t the case, and in fact half of them will die before reaching the mean lifespan. So, when I hear immortalists talking about living to be 120 (or longer) as a result of one or more dietary and/or pharmacological interventions or another, my first thought is, “Shouldn’t you be sure you can crawl before you try to fly?” I say this because, as the data show, it’s not all that easy to make it to “average;” half of those who try die! And if you think about it, why they died (failed) is likely to be very important; even if it was from seemingly random things like a drunk driver hitting them head on, or because they had the misfortune to have the genetic predisposition to type I diabetes.
Table 2. Age-adjusted Death Rates for Various Causes of Death
(per 100,000 population)
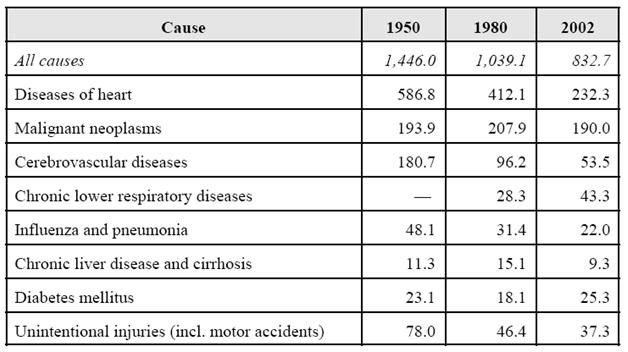
Source: CRS compilation from National Center for Health Statistics (NCHS), Health, United States, 2005 with Chartbook on Trends in the Health of Americans, Table 29.
Of course, most people don’t die from freak accidents; they die from fairly predictable, commonplace and to significant extent avoidable causes, as can be seen in Table 2, above. By far the largest causes of death that prevent people from reaching the statistical mean (or beyond) are cardiovascular disease (CVD) and cancer. To give a better understanding of the percentages, I’ve done a quick and dirty pie chart (Figure 3, below). By far the largest source of theoretically preventable mortality is from cardiovascular disease, and what’s more, interventions that reduce the incidence or severity of CVD also have the potential to reduce the incidence of obesity (in particular, visceral adiposity) and thus the incidence of diabetes. Growing understanding of the biology of atherosclerosis has resulted in dietary interventions, and improved treatment in the form of the statin drugs and coronary revascularization.
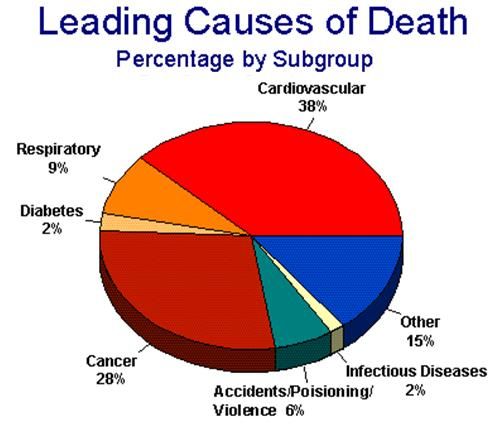 Figure 3: Graphic presentation of the leading causes of mortality in the US as a percentage of all deaths.
Figure 3: Graphic presentation of the leading causes of mortality in the US as a percentage of all deaths.
The first insight into how to prevent, and even reverse atherosclerosis, came in the early 1970s and this insight, and its clinical application have a number of important lessons for today’s ‘do it yourself life extensionists.’
When I arrived in Southern California to work full-time on cryonics in 1974, I stayed for several months with Fred and Linda Chamberlain. I hadn’t been in their home for 24 hours when I was introduced to a book and to a diet that offered the promise of “living to be 100 years old.” The book was titled Live Longer Now and its author, Nathan Pritikin (1915 – 1985), an inventor with no medical background, claimed to have found a diet that would not only prevent atherosclerosis, but also reverse it. I was skeptical at the time, but a decade later I had seen enough firsthand evidence to reconsider Pritkin’s claims. Atherosclerosis most often presents in the form of coronary artery and peripheral artery disease (PAD). While the course is variable in terms of the rate progression, the disease itself is irreversible and by the time it is clinically evident, it has typically been underway for decades.
How not Succeed While Trying: The Pritikin Diet
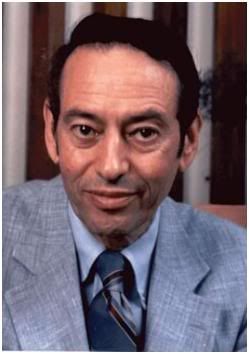 Figure 4: Nathan Pritikin was the classic outsider to medicine. His background was not even that of an academic, but rather that of a successful inventor who made significant contributions to industrial processes in electronics. He was a consummate scientist: a keen observer with an eye for anomalies in the world around him who generated clever hypotheses, and then hammered them into theory using well designed experiments. He was roundly vilified by the medical and scientific communities of the 1970s thru the late 1980s. His theory, that reduction of total serum cholesterol to ~120 mg/dl, and in particular LDL cholesterol to ~<80 mg/dl, in combination with a program of weight reduction and modification of the diet to exclude simple carbohydrates, keep fat consumption to ~ 10% of calories and eliminate added salt is now widely accepted in a medicine. [2-15]
Figure 4: Nathan Pritikin was the classic outsider to medicine. His background was not even that of an academic, but rather that of a successful inventor who made significant contributions to industrial processes in electronics. He was a consummate scientist: a keen observer with an eye for anomalies in the world around him who generated clever hypotheses, and then hammered them into theory using well designed experiments. He was roundly vilified by the medical and scientific communities of the 1970s thru the late 1980s. His theory, that reduction of total serum cholesterol to ~120 mg/dl, and in particular LDL cholesterol to ~<80 mg/dl, in combination with a program of weight reduction and modification of the diet to exclude simple carbohydrates, keep fat consumption to ~ 10% of calories and eliminate added salt is now widely accepted in a medicine. [2-15]
I began to see patients with severe coronary artery disease (CAD) and intermittent claudication (PAD) become symptom free and recover excellent levels of exercise tolerance. That prompted me to contact the Pritikin Longevity Center in Santa Barbara, CA in 1982 and to begin closely looking at the data from the clinical study they were doing at the Veterans’ Administration Hospital in Long Beach, CA on patients with well documented CAD and PAD. Their data were unequivocal; the diet was capable of reducing atheromatous plaques in the coronary arteries, as demonstrated by angiography, as well as reversing ST-segment changes associated with myocardial ischemia during exercise (treadmill testing).
Shortly thereafter, I began advocating (as well as personally practicing) the Pritikin diet to Alcor members, and to cryonicists in general, as a way to avoid the catastrophe of Sudden Cardiac Death (SCD), and possibly to live longer, as well.[16, 17] I learned a number of important things from that experience. The first was that very low fat diets were intensely unpleasant for most people, and that even people who were well aware that they were dying from CAD would either not adopt the diet, or became noncompliant after a short while on it.
The first lesson was thus that an intervention that works is of little use (beyond the mechanistic insights it offers) if no one will use it. I also learned that any claims for life span extension, or improved wellbeing and overall health (for any intervention), must be backed up with data demonstrating those claims. In particular, I learned that all-cause mortality was the last and the best word in validating claims of extending lifespan.
 The Pritikin diet was, in fact, effective at dramatically reducing morbidity and mortality from CVD and type II diabetes.[2, 13, 14, 18-26] However, because the diet eschewed all fats and restricted the calorie intake in fats to 10-15% of the total calorie intake of the diet, with the emphasis on polyunsaturated fats. As previously noted, it proved almost impossible to persuade Alcor members to adopt the diet,[27] or even to embrace a modified version of it, wherein one day a week was a “diet free day,” during which the individual could eat proscribed foods ad lib, as he chose. Somewhat surprisingly, I am still in contact with all six of the surviving individuals who adopted the Pritikin diet between 1974 and 1985; the maximum period of compliance was 6 years, and none of these individuals is still on the diet. Three of these individuals have been treated for cancer, though I would hasten to add that I do not believe that in any of these cases the Pritikin diet was either causative or contributory.
The Pritikin diet was, in fact, effective at dramatically reducing morbidity and mortality from CVD and type II diabetes.[2, 13, 14, 18-26] However, because the diet eschewed all fats and restricted the calorie intake in fats to 10-15% of the total calorie intake of the diet, with the emphasis on polyunsaturated fats. As previously noted, it proved almost impossible to persuade Alcor members to adopt the diet,[27] or even to embrace a modified version of it, wherein one day a week was a “diet free day,” during which the individual could eat proscribed foods ad lib, as he chose. Somewhat surprisingly, I am still in contact with all six of the surviving individuals who adopted the Pritikin diet between 1974 and 1985; the maximum period of compliance was 6 years, and none of these individuals is still on the diet. Three of these individuals have been treated for cancer, though I would hasten to add that I do not believe that in any of these cases the Pritikin diet was either causative or contributory.
Near Universal Noncompliance = Failure
The reasons for the noncompliance, and ultimately for abandonment of the Pritikin diet, were not difficult to ascertain. The most pressing and immediate were the near constant cravings for prohibited foods which, contrary to statement from the Pritikin Longevity Center and those present in Pritikin-approved books and publications, did not diminish over time. Hunger, per se, was not a problem, since the bulk amount of food consumed typically increased over baseline, due to the low caloric density of the foods allowed on diet.[28] Additionally, there were serious problems with mood (irritability and depression), fatigue, reduced ability to concentrate, winter pruritis, binge eating and “constantly feeling cold,” including a much reduced ability to tolerate cool or cold environments when at rest or a low level of activity.[27] There have been no long-term compliance or all-cause mortality studies of the Pritikin diet, however one published study of a nearly identical diet showed very poor compliance at one year.[29]
 Since the mid-1980s, a significant amount of evidence has accumulated indicating that the very low serum cholesterol levels required to effect the reversal of atherosclerosis can result in mood disorders leading to increased irritability, and even violence.[30-36] Studies of more modest reductions in dietary fat intake have not shown benefit in reducing morbidity and mortality from CVD or cancer, and there is the suggestion that mortality reductions resulting from decreases in CVD, hypertension, obesity and diabetes may be made up for by increases in the incidence cancer, suicide and homicide.[27, 31, 37] However, the bottom lines is that 30 years later, there is still no evidence indicating that the Pritikin diet reduces all-cause mortality, or that the non-compliance obstacle can be overcome. The absence of effect with moderate (i.e., less extreme) or so called “reduced fat” diets is especially discouraging, because it indicates the likelihood of an “almost all or none” effect with little or benefit obtained from partial compliance.[38-40] This is, in fact, the position that Nathan Pritikin took.[41]
Since the mid-1980s, a significant amount of evidence has accumulated indicating that the very low serum cholesterol levels required to effect the reversal of atherosclerosis can result in mood disorders leading to increased irritability, and even violence.[30-36] Studies of more modest reductions in dietary fat intake have not shown benefit in reducing morbidity and mortality from CVD or cancer, and there is the suggestion that mortality reductions resulting from decreases in CVD, hypertension, obesity and diabetes may be made up for by increases in the incidence cancer, suicide and homicide.[27, 31, 37] However, the bottom lines is that 30 years later, there is still no evidence indicating that the Pritikin diet reduces all-cause mortality, or that the non-compliance obstacle can be overcome. The absence of effect with moderate (i.e., less extreme) or so called “reduced fat” diets is especially discouraging, because it indicates the likelihood of an “almost all or none” effect with little or benefit obtained from partial compliance.[38-40] This is, in fact, the position that Nathan Pritikin took.[41]
So while the Pritikin diet met Level-1 (Evidence Based Medicine) criteria for reversing atherosclerosis (and in some cases, type II diabetes), it failed to meet the three other claims it made; namely a longer lifespan with the prospect of reaching age 100, greatly reduced incidence of cancer and a healthier happier life as a result of decreased disease burden. Despite its failure as a technique to reduce all-cause mortality,[4] the Pritkin diet was important because it demonstrated for the first time that it was indeed possible not only to prevent or slow atherosclerosis, but to reverse it, as well – and to do so by something as seemingly low technology as dietary intervention. The Pritikin diet was also effective at reversing type II diabetes in many patients, as well as reducing or eliminating the need for antihypertensive medication, especially in patients who were overweight. Despite these formidable advantages, its poor rate of compliance (negligible amongst cryonicists and life extensionists, as well as cardiac patients) and its failure to improve all-cause mortality has made it a practical failure for population-wide application. [5]
Footnotes
[1] One of the best ways to do this is to ask people who are tethered to one spot by work, queuing, or smoking outdoors. Asking people who are waiting in line at a shop or who are workers in shops or restaurants works well as long as your approach is low key, you offer a reasonable explanation for the question and you show genuine interest in their answer.
[2] Life expectancy is a hypothetical measure that applies today’s age-specific death rates to predict the future survival of a cohort. It would technically be more accurate to follow the cohort through time and apply the actual age-specific death rates that the cohort experiences as it moves through its life course, but calculation of actual life expectancy would then require something in excess of 100 years (until the death of the last survivor in the cohort).
[3] Later year estimates are more reliable than those of the early 20th century. The federal civil registration system began in 1900 with the setting up of the Death Registration Area (DRA). States were only admitted as qualification standards were met. Only 10 states and the District of Columbia were in the original DRA of 1900. Statistics prior to 1939-1941 are based on data from the DRA states (which increased in number over time). Alaska and Hawaii are first included in 1959-1961 figures. Also note that data for years 1999-2001 are not reported in this data source.
[4] Absence of evidence is not evidence of absence, but in this case it is strongly suggestive There have been no all cause mortality studies published on the Pritikin diet despite the Pritikin Research Foundation’s heavy emphasis on scientific data to validate claims for the diet. Longitudinal studies of diets require both long term compliance and a study group large enough to draw accurate statistical inferences from.
[5] The Pritikin diet, or its cousin the Ornish diet may still have an important role in the reversal of atherosclerosis in patients who do not wish to undergo coronary artery bypass surgery and who cannot or will not take medication.
References
1. NVSS: National Vital Statistics Reports :http://www.cdc.gov/nchs/data/nvsr/nvsr59/nvsr59_02.pdf. In., vol. 59: Centers for Disease Control and Prevention; 2010.
2. Barnard RJ, Lattimore L, Holly RG, Cherny S, Pritikin N: Response of non-insulin-dependent diabetic patients to an intensive program of diet and exercise. Diabetes Care 1982, 5(4):370-374.
3. Weber F, Barnard RJ, Roy D: Effects of a high-complex-carbohydrate, low-fat diet and daily exercise on individuals 70 years of age and older. J Gerontol 1983, 38(2):155-161.
4. Barnard RJ, Massey MR, Cherny S, O’Brien LT, Pritikin N: Long-term use of a high-complex-carbohydrate, high-fiber, low-fat diet and exercise in the treatment of NIDDM patients. Diabetes Care 1983, 6(3):268-273.
5. Masley S, Kenney JJ, Novick JS: Optimal diets to prevent heart disease. JAMA 2003, 289(12):1510; author reply 1510-1511.
6. Masley SC: Dietary therapy for preventing and treating coronary artery disease. Am Fam Physician 1998, 57(6):1299-1306, 1307-1299.
7. Masley SC, Weaver W, Peri G, Phillips SE: Efficacy of lifestyle changes in modifying practical markers of wellness and aging. Altern Ther Health Med 2008, 14(2):24-29.
8. Barnard RJ, Jung T, Inkeles SB: Diet and exercise in the treatment of NIDDM. The need for early emphasis. Diabetes Care 1994, 17(12):1469-1472.
9. Barnard RJ, Hall JA, Chaudhari A, Miller JE, Kirschenbaum MA: Effects of a low-fat, low-cholesterol diet on serum lipids, platelet aggregation and thromboxane formation. Prostaglandins Leukot Med 1987, 26(3):241-252.
10. Barnard RJ, Ugianskis EJ, Martin DA, Inkeles SB: Role of diet and exercise in the management of hyperinsulinemia and associated atherosclerotic risk factors. Am J Cardiol 1992, 69(5):440-444.
11. Czernin J, Barnard RJ, Sun KT, Krivokapich J, Nitzsche E, Dorsey D, Phelps ME, Schelbert HR: Effect of short-term cardiovascular conditioning and low-fat diet on myocardial blood flow and flow reserve. Circulation 1995, 92(2):197-204.
12. Roberts CK, Barnard RJ: Effects of exercise and diet on chronic disease. J Appl Physiol 2005, 98(1):3-30.
13. Blankenhorn D, Hodis N.: George Lyman Duff Memorial Lecture. Arterial imaging and atherosclerosis reversal. Arteriosclerosis and Thrombosis 1994, 14,:177-192.
14. Hubbard J, Inkeles, S, Barnard, RJ.: Nathan Pritikin’s Heart. N Engl J Med 1985, 313:52.
15. Masley S, Kenney, JJ, Novick, JS.: Optimal diets to prevent heart disease. JAMA 2003, 289(12):1510.
16. Darwin M: Atherosclerosis: answers bring dilemmas: http://www.alcor.org/cryonics/cryonics8412.txt. Cryonics 1984(53):5-8.
17. Darwin MH, SB.: Reducing your risk of autopsy: the problem of atherosclerosis. Cryonics 1987, 8(12):32-47.
18. Barnard R, Pritikin, R, Rosenthal, R, et al.: Pritikin Approach to Cardiac Rehabilitation; Rehabilitation Medicine. St. Louis: Mosby Company, ; 1988.
19. Barnard R, Massey, MR, Cheney, S, O’Brien, LT, Pritikin, N.: Long-term use of a high-complex-carbohydrate, high-fiber, low-fat diet and exercise in the treatment of NIDDM patients. Diabetes Care 1983, 6:268-273.
20. Barnard R, Guzy, J, Rosenberg, LT, et al. : Effects of an intensive exercise and nutrition program on patients with coronary artery disease: a five-year follow-up. J Cardiac Rehab 1983, 3:183-190.
21. Ornish D, Scherwitz LW, Billings JH, Brown SE, Gould KL, Merritt TA, Sparler S, Armstrong WT, Ports TA, Kirkeeide RL et al: Intensive lifestyle changes for reversal of coronary heart disease. JAMA 1998, 280(23):2001-2007.
22. Ornish D, Brown SE, Scherwitz LW, Billings JH, Armstrong WT, Ports TA, McLanahan SM, Kirkeeide RL, Brand RJ, Gould KL: Can lifestyle changes reverse coronary heart disease? The Lifestyle Heart Trial. Lancet 1990, 336(8708):129-133.
23. Ornish D: Reversing heart disease through diet, exercise, and stress management: an interview with Dean Ornish. Interview by Elaine R Monsen. J Am Diet Assoc 1991, 91(2):162-165.
24. Ornish D: Can lifestyle changes reverse coronary heart disease? World Rev Nutr Diet 1993, 72:38-48.
25. Gould KL, Ornish D, Scherwitz L, Brown S, Edens RP, Hess MJ, Mullani N, Bolomey L, Dobbs F, Armstrong WT et al: Changes in myocardial perfusion abnormalities by positron emission tomography after long-term, intense risk factor modification. JAMA 1995, 274(11):894-901.
26. Gould KL, Ornish D, Kirkeeide R, Brown S, Stuart Y, Buchi M, Billings J, Armstrong W, Ports T, Scherwitz L: Improved stenosis geometry by quantitative coronary arteriography after vigorous risk factor modification. Am J Cardiol 1992, 69(9):845-853.
27. Gittleman A: Beyond Pritikin: A Total Nutrition Program For Rapid Weight Loss, Longevity, & Good Health: Bantam; 1988.
28. Freedman M, King, J, Kennedy, G.: Popular Diets: A Scientific Review : http://www.nature.com/oby/journal/v9/n3s/pdf/oby2001116a.pdf. Obesity Research 2001, 9(Suppl 1):1-40s.
29. Thuesen L, Henriksen, LB, Engby, B.: One-year experience with a low-fat, low-cholesterol diet in patients with coronary heart disease. Am J Clin Nutr 1986, 44::212-219.
30. Golomb BA, Stattin H, Mednick S: Low cholesterol and violent crime. J Psychiatr Res 2000, 34(4-5):301-309.
31. Kaplan JR, Muldoon MF, Manuck SB, Mann JJ: Assessing the observed relationship between low cholesterol and violence-related mortality. Implications for suicide risk. Ann N Y Acad Sci 1997, 836:57-80.
32. Wallner B, Machatschke IH: The evolution of violence in men: the function of central cholesterol and serotonin. Prog Neuropsychopharmacol Biol Psychiatry 2009, 33(3):391-397.
33. Golomb BA, Kane T, Dimsdale JE: Severe irritability associated with statin cholesterol-lowering drugs. QJM 2004, 97(4):229-235.
34. Rose N, Koperski S, Golomb BA: Mood food: chocolate and depressive symptoms in a cross-sectional analysis. Arch Intern Med, 170(8):699-703.
35. Ainiyet J, Rybakowski J: [Low concentration level of total serum cholesterol as a risk factor for suicidal and aggressive behavior]. Psychiatr Pol 1996, 30(3):499-509.
36. Fawcett J, Busch KA, Jacobs D, Kravitz HM, Fogg L: Suicide: a four-pathway clinical-biochemical model. Ann N Y Acad Sci 1997, 836:288-301.
37. Wells A, Read, NW, Laugharne, JDE, Ahluwalia, NS. : Alterations in mood after changing to a low-fat diet. British Journal of Nutrition 1998, 79:23-30.
38. Krauss R: Low-fat dietary pattern and risk of cardiovascular disease in the Women’s Health Initiative Randomized Controlled Dietary Modification Trial. Curr Atheroscler Rep 2007, 9(6):431-433.
39. Prentice RL, Caan B, Chlebowski RT, Patterson R, Kuller LH, Ockene JK, Margolis KL, Limacher MC, Manson JE, Parker LM et al: Low-fat dietary pattern and risk of invasive breast cancer: the Women’s Health Initiative Randomized Controlled Dietary Modification Trial. JAMA 2006, 295(6):629-642.
40. Tinker LF, Bonds DE, Margolis KL, Manson JE, Howard BV, Larson J, Perri MG, Beresford SA, Robinson JG, Rodriguez B et al: Low-fat dietary pattern and risk of treated diabetes mellitus in postmenopausal women: the Women’s Health Initiative randomized controlled dietary modification trial. Arch Intern Med 2008, 168(14):1500-1511.
41. Leonard J, Hofer, JL, Pritikin, N.: Live Longer Now: Grosset & Dunlap; 1974.

It seems that average life expectancy is a tricky concept for many. Life expectancy DOES NOT equal mean lifespan. In 2007 US life expectancy stood at 78.3 yet the age that 50% are expected to reach were 82.2 years (mean lifespan). Life expectancy is always distorted by early-life mortality. Around 60% reach the life expectancy age. Do not confuse average with mean.