By Mike Darwin
CPB at BPI
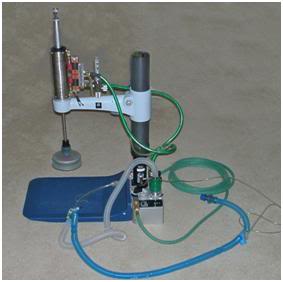
When I left Alcor and started BioPreservation, Inc., (BPI) in 1992, the same high standard of care was continued. Where there was adequate notice, cardiopulmonary bypass (CPB) was initiated in the home using mechanical cardiopulmonary support (CPS) as a bridge, and the quality of CPS was greatly improved by combining active compression-decompression CPS (ACD-CPS) with high impulse chest compressions. Again, Michigan Instruments was enlisted to build a pneumatically powered machine that could deliver this modality, and which could also eliminate the pauses in chest compression (and thus interruptions in blood flow), required to administer ventilations.37
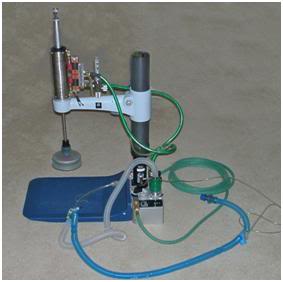 Figure 45: Active Compression-Decompression High Impulse CPS machine first put into clinical application on 12 Dec 1995.
Figure 45: Active Compression-Decompression High Impulse CPS machine first put into clinical application on 12 Dec 1995.
In-home CPB was continued until BioPreservation ceased operations in 1996.38 The original ECMO[1] cart developed by Jerry Leaf had many modifications and improvements added to it by the time it was retired, including a CDI monitor for continuous in-line arterial and venous pH and blood gases, a computerized ACD-HI CPS machine, and increased battery life and oxygen carrying capacity (see Figures 46 & 47, below).
 Figure 46: MALSS being set up in a patient’s living room for in-home CPB on 12 December, 1995.
Figure 46: MALSS being set up in a patient’s living room for in-home CPB on 12 December, 1995.
 Figure 47: Patient undergoing in-home CPB following immediate post arrest support with ACD-HI CPS.
Figure 47: Patient undergoing in-home CPB following immediate post arrest support with ACD-HI CPS.
In cases where the patient was remote from BPI’s facilities in Southern California, and where in-home CPB[2] was possible, a Remote Standby capability was deployed. BPI maintained two fully equipped ambulances as well as two complete Remote Standby kits fully stocked with all of the hardware and consumables required to initiate CPB, as seen in Figures 48 and 49, below.39

Figure 48: CPB set-up deployed in the home of long time cryonicist and cryopatient Jerry White, in Northern California. Jerry was cryopreserved on 05 February, 1994.

Figure 49: Extracorporeal circuit and portable ice bath in position in Jerry White’s condominium in February of 1994.
As was the case during my time at Alcor, cryoprotective (CPA) perfusions at BPI continued to be carried out using standard extracorporeal technology with virtually all of the perfusion and monitoring equipment used having been made by well respected medical manufacturers.40-42
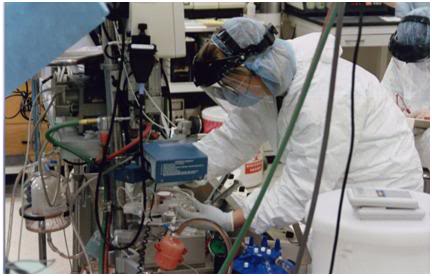 Figure 50: Experienced experimental animal perfusionist from UC Davis Veterinary School (under contract to BPI) withdrawing a perfusate sample for analysis during the cryoprotective perfusion of Jerry White in 1994.
Figure 50: Experienced experimental animal perfusionist from UC Davis Veterinary School (under contract to BPI) withdrawing a perfusate sample for analysis during the cryoprotective perfusion of Jerry White in 1994.

Figure 51: Cryoprotective perfusion tableaux at BPI in 1994.
 Figure 52: Cryoprotective perfusion circuit used for Jerry White at BPI in 1994. The only ‘non-medical’ pieces of equipment in the circuit are the perfusate reservoirs, and the magnetic stir stable and stir bar, used to mix the CPA concentrate with the recirculating perfusate; a requirement unique to human cryopreservation operations.
Figure 52: Cryoprotective perfusion circuit used for Jerry White at BPI in 1994. The only ‘non-medical’ pieces of equipment in the circuit are the perfusate reservoirs, and the magnetic stir stable and stir bar, used to mix the CPA concentrate with the recirculating perfusate; a requirement unique to human cryopreservation operations.
The same was true of the surgical instruments and cannulae used for cryoprotective perfusion. My philosophy was, from the beginning, not to re-invent the wheel and, wherever possible, to use existing hardware and existing technology. Aside from the commonsense and practical reasons inherent in such an approach, it offered the incalculable advantage of allowing me and my colleagues more time to spend on solving problems not yet solved, and, where necessary, to fabricate novel hardware for which there was a pressing need – but no supplier.
 Figure 53: Some of BPI’s cardiothoracic instruments on the back table during the cryopreservation of Richard Marsh at BPI on 06 May, 1994.
Figure 53: Some of BPI’s cardiothoracic instruments on the back table during the cryopreservation of Richard Marsh at BPI on 06 May, 1994.
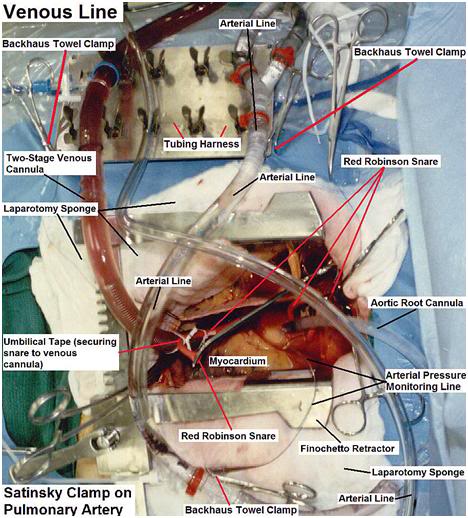 Figure 54: Cannulae and tubing configuration (median sternotomy) employed at BPI (cryopreservation of Richard Marsh on 06 May, 1994).
Figure 54: Cannulae and tubing configuration (median sternotomy) employed at BPI (cryopreservation of Richard Marsh on 06 May, 1994).
 Figure 55: Board Certified clinical perfusionist performing the cryoprotective perfusion of Richard Marsh at BPI on 06 May, 1994.
Figure 55: Board Certified clinical perfusionist performing the cryoprotective perfusion of Richard Marsh at BPI on 06 May, 1994.
One of the more bizarre fixations to emerge in the recent criticism of cryonics is the notion that cryonicists have had no contact with extracorporeal medicine or professional Board Certified perfusionists. Nothing could be further from the truth. The first perfusions carried out at Cryovita were pumped by a Board Certified Perfusionist who was a former colleague of Jerry Leaf’s. This allowed Jerry to concentrate his efforts on surgery to cannulate the patient and prepare him for connection to the extracorporeal circuit. Jerry was himself a Board eligible perfusionist, with countless clinical hours, in addition to his research CPB experience; he was the primary perfusionist at the UCLA cardiothoracic surgery research laboratory, and he was a skilled ‘surgeon’ who instructed clinical cardiothoracic surgeons at UCLA during their residencies.
I put apostrophes around the word surgeon when using it to describe Jerry Leaf; because it has recently been has implied that the use of this word to describe the position of the person who performs ‘surgery’ on cryopatients constitutes ‘practicing medicine without a license’[3] and ‘misleading or defrauding the public by projecting an image of medical certification and licensure.’ Of course, nothing could be further from the truth, and both Jerry and I were always careful to state who and what we were – including the absence of doctorates, medical degrees, or professional certifications. In particular, I have been accused of passing myself off as a ‘nurse,’ and to have otherwise misrepresented my qualifications. This is a lie, pure and simple, and I have never advertised, nor allowed to stand, any notion than I am anything other than a secondary school educated man with 3 months of additional training as a hemodialysis technician.
I have also been ruthlessly honest about the near absence of my math skills (and abilities) and have been blunt that this defect alone would have precluded me from ever obtaining a Ph.D. in any science, let alone an M.D. While I wish I could have been better formally educated, I am very proud of what I have achieved absent a university degree, and I am very glad I persisted in my pursuit of the sciences. My achievements are what they are, and they have been extensively documented in writing; and most of that work is available on the Internet today. The reader may access these materials and judge for himself to what extent my work has merit.
Similarly, BPI employed two perfusionists: one a practicing Board Certified clinical perfusionist, and the other a highly skilled and very experienced research and clinical veterinary perfusionist who had trained and worked at the UC Davis School of Veterinary Medicine. One of these perfusionists was present at every case BPI pumped. Going beyond perfusion, it should be noted that both Jerry Leaf and I were, in cryonics terms, very successful at recruiting people into our cryopreservation teams who were licensed biomedical professionals.
At any one time, the teams had an RN, LVN, perfusionist, Medical Technologist, Respiratory Therapist or physician (and usually combinations of the aforementioned). Dr. Thomas Munson, now a patient at Alcor, was a physician-surgeon with many years of experience who scrubbed in on almost all Alcor cases from shortly after the time he was recruited as a member from a lecture I gave in San Diego, until (at least) after I left Alcor in 1991. Dr. Steve Harris, who became involved in cryonics after I contacted him about an article he had written in regard to aging in the early 1980s, was also a great source of expertise, and was not infrequently present at Alcor cryopreservations. One young man who literally showed up on our doorstep, Scott Greene, put himself through EMT[4] training and then worked as an EMT while he put himself through nursing school (he often had two jobs at a time). Scott was an integral and highly valued member of the team until I left, and he took work as an RN at far remove from Colton, CA where BPI was first located.
BPI and Alcor also employed several highly skilled professionals who were not directly involved in human medicine, but who were uniquely (indeed enviably) qualified to participate in cryonics cases. One of these was a veterinary cardiothoracic surgeon who made his living, in part, by implanting novel prosthetic heart valves, left ventricular assist devices (LVADs) and total artificial hearts (TAHs) in sheep and cattle for long-term evaluation prior to human clinical trials. He was a superb cardiac surgeon and perfusionist with an enormous reservoir of experience – he had even done some of the chronic implants of the Jarvik TAH in calves. These people did not want to be publicly associated with cryonics for reasons that anyone who has read these recent attacks should readily be able to appreciate.
Finally, a word of caution: When confronted with evidence that is contrary to their stated opinions or conclusions, these critics have, in the past simply denied or redefined that evidence. A case in point is the photograph shown in Figure 56, below. This photo was originally included in a report that a former perfusionist who worked at Suspended Animation, Inc., received a copy of during her employ there. She subsequently stated on the Cold Filter cryonics discussion forum that this photo showed the presence of air in the extracorporeal circuit, in particular in the pump ‘shoe’ or raceway. If this was indeed the case, it would be indicative of gross incompetence on the part of the perfusionist – who in this case happened to be me.
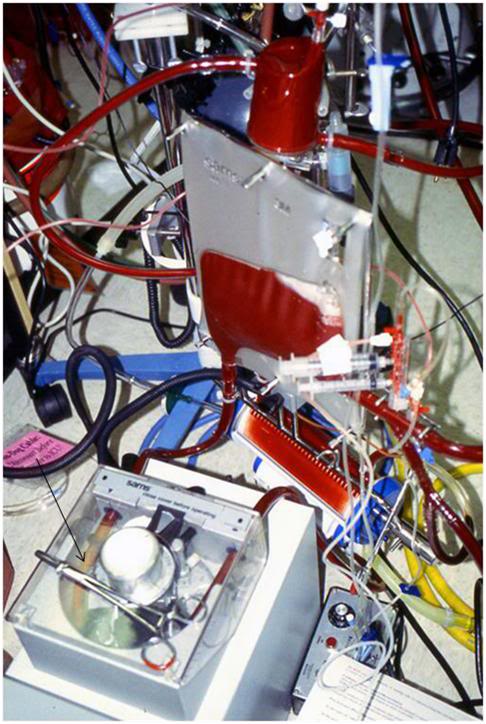
Figure 56: Pump raceway showing serum separation from blood (arrow) following termination of active cardiopulmonary support in a canine resuscitation dog experiment conducted at 21st Century Medicine in the late 1990s.
I tried to point out that she was mistaken in her assertion, and that what she was stating was air, was in fact separation of the red cells from the serum due to sedimentation of the cells under the force of gravity. This could (and did) occur because the pump was shut off, and had been shut off for some time. In this model the animals were severely vasoconstricted at the conclusion of the period of post-ischemic extracorporeal support due to the administration of vasopressin, and it was not possible to return much of the blood present in the extracorporeal circuit until many minutes after the animal was weaned from the pump. As a consequence, blood remained in the extracorporeal circuit and was gradually re-infused into the animal as the vasopressin was metabolized, and the vasoconstriction subsided. During this period, red cells fall to the more dependant part of the circuit under the influence of gravity. This sedimentation of red cells was further enhanced by the presence of therapeutic drugs that elevated the sedimentation rate.
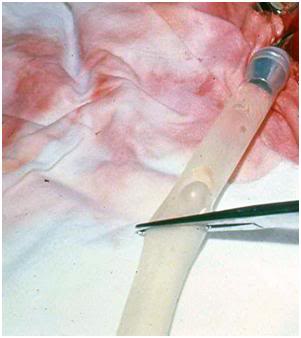 Figure 57: Air bubble in silastic tubing during cryoprotective perfusion of a cryopatient in 1975. The high surface tension of water causes the bubble to have spherical contours as consequence of its interaction with air at the air-liquid interface.
Figure 57: Air bubble in silastic tubing during cryoprotective perfusion of a cryopatient in 1975. The high surface tension of water causes the bubble to have spherical contours as consequence of its interaction with air at the air-liquid interface.
In point of fact, it is a bit surprising that a perfusionist, whose attitude and remarks would appear to indicate she is all knowing on any subject related to CPB, would not know that water has enormous surface tension, and thus water-air (or blood-air) interfaces exhibit a meniscus, as can be seen in Figure 57, above. Not only is there no meniscus in the tubing in Figure 56, close inspection reveals that sedimentation is also underway (though much less complete) on the side of the tubing raceway that is on the opposing side to where it was asserted there was a large amount of air present (i.e., the right side). Yellow tinged serum can be seen to be appearing in this tubing; although the degree of red cell sedimentation is not as pronounced.
To sum up, this new generation of cryonics ‘critics’ has no sincere interest in improving cryonics, or in helping cryonicists. It is unfortunate that the first contact with cryonics for some of these individuals has been with utterly incompetent practitioners of cryonics. Much of the criticism of SA that been leveled at the operation during the period of (at least) 2006-7 were, in my opinion, valid – and I say this based on firsthand experience as an unpaid consultant to SA in 2006. However, it is even more unfortunate that these critics went no further, and that they have based their evaluation of the use of extracorporeal technology in cryonics during the period from 1981 to 1995, as practiced by Jerry Leaf and I, based on their adverse experience with institutions where neither Jerry or I had any authority or responsibility.
This in no way constitutes an excuse for their indiscriminate reign of terror – indeed, my first experience of perfusion in cryonics was unarguably vastly more shocking and at variance with anything even remotely resembling medicine. I could have responded with irrational and non-constructive criticism, but instead, I responded by documenting what I found and putting forth every bit of effort I could muster to change things for the better. And above all, when I had the good fortune to encounter others in cryonics that were both competent and committed to doing the same, I had the good sense to set my ego aside and go to work with them in attempting to make cryonics into a scientifically rigorous and professionally accountable discipline.
The End
References
37) Darwin, M. A new kind of CPR. CryoCare Report #2 online edition, July 1994: http://www.cryocare.org/index.cgi?subdir=&url=ccrpt2.html#GUIDELINES. Retrieved 2011-01-24.
38) Darwin, M. Cryopreservation of James Gallagher, CryoCare patient #C-2150: http://www.alcor.org/Library/html/casereportC2150.htm. Retrieved 2011-01-29.
39) Darwin, M. Cryopreservation case report: Jerome Butler White, http://cryoeuro.eu:8080/pages/viewpageattachments.action?pageId=425990&sortBy=date&highlight=White_Jerome_Butler_Case_Report.pdf&. Retrieved 2011-01-30.
40) Darwin, M. Cryopreservation case report: Richard Putnam Marsh, ACS 5694. http://cryoeuro.eu:8080/pages/viewpageattachments.action?pageId=425990&sortBy=date&highlight=Marsh%2C+Richard+P.+Cryopreservation+Summary.pdf&. Retrieved 2011-01-30.
41) Darwin, M. Cryopreservation of James Gallagher, CryoCare patient #C-2150: http://www.alcor.org/Library/html/casereportC2150.htm. Retrieved 2011-01-29.
42) Darwin, M. Cryopreservation case report: Jerome Butler White, http://cryoeuro.eu:8080/pages/viewpageattachments.action?pageId=425990&sortBy=date&highlight=White_Jerome_Butler_Case_Report.pdf&. Retrieved 2011-01-30.
[1] Extracorporeal Membrane Oxygenation (ECMO).
[2] Cardiopulmonary bypass (CPB).
[3] Of course, one problem with this charge is that our patients are legally dead. It is only possible to practice medicine on legally dead people under special circumstances, such as performing a medico-legal autopsy.
[4] Emergency Medical Technician (EMT)

3D News
I love this particular web site, lots of instances I check out internet sites and they are simply filled with junk. But, this is real quality
Thanks, but please, tell me what you find valuable about it? – Mike Darwin
I find this very interesting and from what I have read, is an up front, honest account about what has/is going on. I have been a certified perfusionist for over 20 years and anyone “worth their salt” so to speak in the profession would know that this was not air in the raceway boot but, was indeed exactly as described. Sedimentation occurs in various areas of the perfusion circuit if there is no movement. The only things I can really think of why “their indiscriminate reign of terror” exists is because of ignorance, a religious component and the fact that they were made to look… well, ignorant with religion being the biggest factor as it is in almost everything.
Keep up the good work and as we all know, the discovery of new techniques and ways of doing things takes a huge amount of time and effort.
Thanks for your comment; you are the first perfusionist, or for that matter, the first in any medicine-related discipline to comment. I don’t think Ms. Maxim’s actions had any roots in religion. She was hired to work as a perfusionist for a cryonics company in South Florida. Unfortunately, her experience there was not positive. In fact, much of her early criticism of perfusion in cryonics was either valid, or had some basis in fact. I spent ~ 5 days at this enterprise shortly before she was hired, and I can honestly say it was one of the weirdest experiences in my professional life – and coming from me – that’s saying something.
The practice of “perfusion” in cryonics has mostly been incompetent: and by that I mean riddled with iatrogenic events, such pumping air, having aortic root cannulae “pop out” during perfusion, subjecting a patient to a wall water leak through a disposable heat exchanger, and on and on. More recently, competent board certified percussionists are being used in the absence of a competent team leader – the equivalent of the perfusionist functioning in the complete absence of a cardiothoracic surgeon, or an appropriately trained interventional cardiologist. They are, in effect, presented with a cryonics patient and told to “perfuse him.” Missing from that equation are a careful pre-perfusion work-up and a thorough understanding of the possible complications or contraindications that might arise from the patient’s pre-cardiac arrest medical condition. Ditto any deep understanding of the physiology of perfusion under conditions of ultraprofound asanguineous hypothermia, let alone when cryoprotectants are present.
Interestingly, one of the things which outraged Ms. Maxim was my questioning her recommendations for the perfusion of cryonics patients. One of my concerns, which was unheeded, was the damaging effect of ethylene glycol and especially dimethylsulfoxide (DMSO) on polycarbonate, buna-N and PVC components in the circuit. Recently, I read a case account from the Cryonics Institute, who was following Ms. Maxim’s advice and reusing their centrifugal pump heads, that they experienced pump head failure during a case which they attributed to DMSO-induced degradation.
There are many, many such factors unique to the practice of perfusion in cryonics. This is pretty much what should be expected, since the conditions are so radically different than those seen in the clinic (i.e., long ischemic times, depth and duration of hypothermia, effects of cryoprotectant agents, etc.). My comments were not well received and Ms. Maxim seemed fixated on cryonics as medical fraud. Bad practice? There’s certainly plenty of that to go around, but fraud? Well, that requires that the people paying for the bad practice are being deliberately deceived. In fact, they know quite well what he state of affairs is – they simply don’t care – or don’t care enough to change it. — Mike Darwin
I HAVE ALWAYS BEEN FASCINATED BY THIS. IT’S REAL, VALID AND LIKE ROUTINE PERFUSION HAS TO BE MANAGED WITH A PROCESS AND GOAL IN MIND. I HAVE THE FIRST CLINICAL EXPERIENCE OF INDUCING SIGNIFICANT HYPERTHERMIA THERAPEUTICALLY (43.5 DEG C) AND ALWAYS WANTED TO EXPLORE THIS. I ALSO HAVE SUCCESSFULY RESUSCITATED MILITARY PERSONNEL WHO WERE SUFFERING SEVERE HYPOTHERMIA (<22 DEG C). WHAT IS THE STATUS AND WHERE IS THIS BEING DONE IN 2013?