The Urgent Need for a Brain Centered Approach to Geroprotection for Cryonicists
By Mike Darwin

SENIOR MOMENTS
Interestingly, and perhaps somewhat hopefully, the decay of PP axons seems confined largely to two of the nine circuits in this system, as shown in Figure11. It is the two circuits that connect layer II of the entorhinal cortex with the dentate gyrus and the CA3 neurons that appear to be degrading with aging, beginning around age 40. Work by Yassa, et al., published in May of last year, has shown that the extent of decay in the PP correlates well with poor performance in delayed recall in cognitive testing of patients who were imaged in their study of PP microstructure deterioration using a word-list learning task sensitive to defects in hippocampal function.55
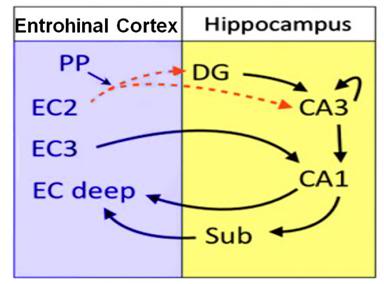 Figure 11: Schematic of the of hippocampal connectivity circuits showing the perforant pathway (PP), entorhinal cortex layer II (EC2,); entorhinal cortex layer III (EC3); deep, entorhinal cortex deep layers (EC); dentate gyrus (DG); subiculum (Sub). The broken red lines emphasizes that these pathways are decaying as a consequence of ‘normal’ aging.
Figure 11: Schematic of the of hippocampal connectivity circuits showing the perforant pathway (PP), entorhinal cortex layer II (EC2,); entorhinal cortex layer III (EC3); deep, entorhinal cortex deep layers (EC); dentate gyrus (DG); subiculum (Sub). The broken red lines emphasizes that these pathways are decaying as a consequence of ‘normal’ aging.
This work also goes a long way towards explaining the onset of difficulty in recall which occurs in many people starting around early middle age, and which typically becomes progressively more problematic in the decades that follow. For many people, by the time they reach their mid-50s to mid-60s, they are experiencing frustrating ‘word searching’ and the inability to recall well known facts or names – only to have the sought for information ‘come to mind,’ or even days later. This kind of hippocampal output failure is consistent with the deterioration in micromorphology now being discovered in PP axons in middle aged and older humans, and mirrors the same structural and cognitive declines in this pathway that have been observed in rodents.
CORRELATION BETWEEN STRUCTURAL CHANGES AND FUNCTIONAL COGNITIVE DECLINE
The prefrontal cortex and underlying white matter are the last areas of the brain to complete myelination and to reach their maximum volume and, presumably, cell density. They are also the first white matter areas of the cerebral cortex to begin to undergo neurodegeneration. Myelination of the frontal cortex typically isn’t completed until the early to mid 20s, and its relentless degeneration begins essentially upon the completion of its development. This more or less linear degradation of the prefrontal and medial temporal lobe white matter correlates with slowed processing speed initially and, later in life, with declines in all areas of cognition.56
The impact of this structural degeneration on cognitive performance in most areas of intellectual processing is not usually apparent until the mid 50s; many abilities such as verbal fluency continue to increase until the mid 50s or even the early 60s.57 While there is linear brain matter loss with increasing age, specific anatomical areas of the brain degenerate at different rates, with some areas exhibiting volume increases into the mid 50s, after which virtually all areas of the neocortex undergo relentless degeneration (including lesioning, as well as volume loss) until death occurs. There is also considerable variation amongst individuals which appears to occur independent of any discrete pathological processes.58
Paradoxically, the fact that this neurodegeneration is occurring is masked to a large degree by several compensatory mechanisms that preserve overall function, as we shall soon see. This leads to a nearly universal attitude of denial in most aging people who continue to insist, often into their 60s and 70s that they (presumably unlike all the others of their species) are being spared meaningful cognitive decline – and in fact may be intellectually ‘sharper’ as they age, as opposed to actually losing neurocognitive ability.[1] There is a good reason for this omnipresent delusion and that is that even though cognitive performance starts to seriously decline, on average, in the mid 50s, a few cognitive domains increase between age 25 and age 55; thus, the declines in late life often merely bring cognitive performance back down to where it was in the mid 20s. Of course, processing speed in late life is vastly slower than it was when it peaked in the 20s, but verbal memory and abilities, reasoning, and spatial abilities are generally well preserved into late life.59
The devastating impact of the loss of raw processing power is best seen in the absolute decline in mathematical abilities, which decrease relentlessly over the course of a human life span. The graphs in Figure 12 show cognitive performance, as measured by the Seattle Longitudinal Study, a 35-year long longitudinal study (actually a sequential research design – both cross-sectional and longitudinal). As can be seen in Graph A, cross-sectional analysis of data from the study demonstrate that cuts are evident in all cognitive domains in aging, with the exception of preserved verbal and numeric ability. Graph B shows the longitudinal data which demonstrate that declines occur in all cognitive domains after age 55.
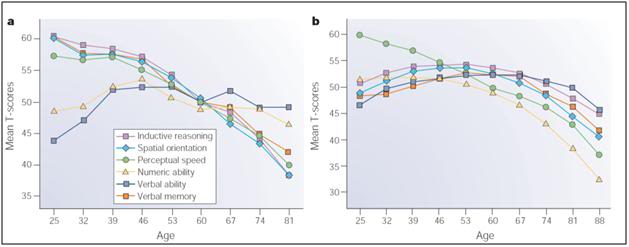 Figure 12: Cross-sectional and longitudinal estimates of age-related change in cognition. A) Cross-sectional data from the Seattle Longitudinal Study. Declines are evident in all domains, with the exception of preserved verbal and numeric ability. B) Seven year longitudinal data from the same study. Declines are evident in all domains after age 55, with only processing speed displaying declines before 55. These graphs graph shows cognitive performance as measured by a 35-year longitudinal study (actually a sequential research design – both cross-sectional and longitudinal) [Schaie, K. W. Intellectual Development in Adulthood: The Seattle Longitudinal Study. Cambridge Univ. Press, Cambridge, 1996.]
Figure 12: Cross-sectional and longitudinal estimates of age-related change in cognition. A) Cross-sectional data from the Seattle Longitudinal Study. Declines are evident in all domains, with the exception of preserved verbal and numeric ability. B) Seven year longitudinal data from the same study. Declines are evident in all domains after age 55, with only processing speed displaying declines before 55. These graphs graph shows cognitive performance as measured by a 35-year longitudinal study (actually a sequential research design – both cross-sectional and longitudinal) [Schaie, K. W. Intellectual Development in Adulthood: The Seattle Longitudinal Study. Cambridge Univ. Press, Cambridge, 1996.]
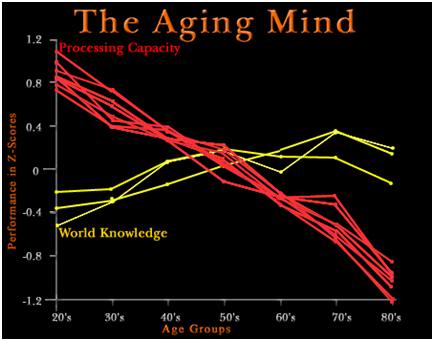
Figure 13: Compensation for neurodegeneration as a result of life-experiences and learning, as well as physiological compensation within the aging brain itself, as illustrated by the increase in word knowledge over the course of the life span.
At least one reason why these enormous functional cuts are not more apparent, or more devastating to individual functioning, is shown in Graph 13. If word knowledge is used as a marker for life experience and the general accumulation of knowledge, then it becomes apparent that knowing more and having more ‘wisdom’ act to offset some of the losses in processing power. Wisdom, as opposed to knowledge or skill, is likely of particular importance, since wisdom is a complex integration of knowledge with emotional learning and divergent life experiences. The difference between knowledge and wisdom can perhaps best be appreciated by an adult telling a child not to play in traffic, or engage in hazardous behavior, at which point the child has the knowledge, but very likely lacks the wisdom (based on repeated, robust, and emotionally charged experiences) to refrain from such behavior.
There are also compensatory changes in the brain itself in terms of how it utilizes its increasingly diminishing processing resources. For instance, it is well established that there is a generalized, age-related reduction of activity in the occipital cortex as a result of the deterioration of sensory processing. Concurrently, there is also an age-related increase in pre-frontal cortex activity, in an attempt to compensate for these deficits.60-63 This relationship between declining occipital function and sensory deficits is consistent with abundant evidence that perceptual processing declines as a function of aging.64 These declines in occipital cortical function have been documented across many different kinds of visual-spatial tasks and support the view that sensory decline is a major factor in cognitive aging.65
Those with a ‘glass half full’ approach to brain aging will point to the data in Figure 13 and cheerfully exclaim “Brain aging isn’t all that bad – life has it compensations, and whilst your brain is deteriorating with age, you are also becoming wiser, and that offsets some of the losses.” This attitude begs the unasked (and unanswered) question, namely, “What would the cognitive performance of the aging or aged human be if there were no accompanying age-associated neurodegeneration?” That graph has not yet been prepared[2], but the answer should be obvious: people would be vastly smarter and more capable as they aged, as opposed to barely holding their own in just a few domains of cognitive performance, while continuing to deteriorate in most others.
An outstanding and highly accessible paper documenting and integrating the structural and functional deterioration of cognition in aging is, Hedden T, Gabrieli JD. Nat Rev Neurosci. 2004 Feb;5(2):87-96. Insights into the aging mind: a view from cognitive neuroscience. PMID 14735112, which is available as full text from this link: http://brainybehavior.com/blog/wp-content/uploads/2007/11/agingbrain.pdf. I cannot recommend this paper highly enough. Additionally, the Salt Cognitive Aging Laboratory, which oversees the Virginia Cognitive Aging Project (VCAP) at the University of Virginia, is the premier facility in the US (and arguably the world) undertaking active, longitudinal studies of aging. The VCAP study has done comprehensive cognitive assessments in adults ranging from 18 to 98 years of age. Approximately 3,800 adults have participated in their three-session (6-8 hour) assessment at least once, with about 1,600 participating at least twice, and about 450 of them participating three or more times. The data from this project have served as the basis for a veritable cornucopia of scientific publications which are available in the Resources Section of their website http://faculty.virginia.edu/cogage/links/publications/. Nearly 200 papers on the cognitive impact of aging are available free of charge on their website. It is necessary to register with your name and email address to access the papers, but it is well worth it. This reservoir of data would take countless hours of on-line research to gather, and many thousands of dollars to download from the web sites of the respective publishers of these papers.
BRAIN MASS LOSS VERSUS BRAIN CELL LOSS
Of course, MRI has its limits as well, and the most important of these in this context is that this imaging technology still cannot resolve individual brain cells. To do that in living humans we are reliant upon light microscopy of brain tissue taken at autopsy, or during neurosurgical procedures that excise a portion(s) of (or biopsy) the brain. This inability to image brain cells is important, because loss of brain volume does not necessarily equate to loss of brain cells. A passable analogy might be that of the skeletal muscles, which can vary enormously in volume and mass, depending upon an individual’s health and conditioning. A professional bodybuilder has roughly the same number of muscle cells after he has ‘bulked up,’ as he did before he began his regimen of exercise (and typically, performance enhancing drugs, as well). The number of muscle cells hasn’t changed, but their volume and character has, and dramatically so.
CLUES FROM DEPRESSIVE DISORDERS
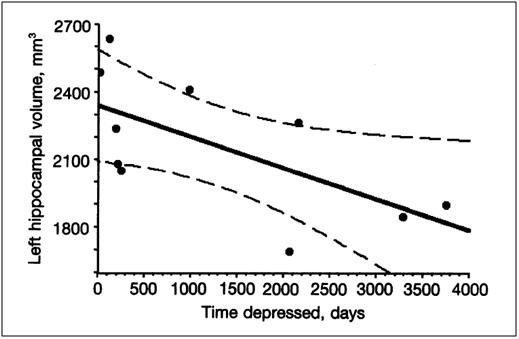
Figure 14: Loss in hippocampal volume as a function of days of major depression experienced. Jang, SW, Liu, X, Chan, CB, Weinshenker, D, Hall, RA, Xiao, G, Ye K. Amitriptyline is a TrkA and TrkB receptor agonist that promotes TrkA/TrkB heterdodimerizat heterdodimerization and has potent neurotrophic activity. Chemistry and Biology, 2009;16, x-y.
Over the past decade there has been a revolution in our understanding of depressive disorders (Major Depressive Disorder, Dysthymic Disorder and Bipolar Disorder) and oddly enough, this may be of considerable relevance to the aging brain. Since the discovery of a class of drugs called the tricyclic antidepressants, of which amitryptyline (Elavil) was the prototypical drug, there has been a great deal of puzzlement over exactly how these drugs work.67 This mystery was deepened when the Serotonin Reuptake Inhibitor (SSRI) drugs were introduced in the 1980s, fluoxetine (Prozac) being the first.68 The first and most evident effect of the SSRIs is to raise the level of serotonin in the brain by inhibiting its reuptake after being released by neurons during neurotransmission. Serotonin is a neurotransmitter – a chemical messenger that acts as a signaling molecule between brain cells — and it is critically involved in regulating mood and appetite, among other things.69
The SSRIs rapidly elevate serotonin levels – in fact they do so within a day or two of the initiation of treatment. Paradoxically, depressed patients who genuinely respond to the drugs (rather than to the placebo effect), do not experience improvement until ~2 weeks, and often much longer, after starting SSRI treatment, or treatment with most other antidepressant drugs, for that matter. There is now substantial evidence that the effect of the SSRIs, and of elevated brain serotonin levels, is to stimulate the release of brain cytokines, which promotes neuronal survival and inhibit aopotosis.70
One thing depressed people do with increased frequency that makes understanding the pathophysiology of their illness considerably easier, is to commit suicide. If there is any up-side to this otherwise disastrous act, it has been that the high suicide rate (~9% vs. 1% in the general population)71– across all three types of depression – has provided researchers with the brains of human sufferers of these illnesses to examine, using a variety of increasingly sophisticated techniques, including histochemistry, and advanced methods of microscopy. The findings from these studies have been as startling as they were unexpected. Without exception, the brains of people suffering from long-standing depressive disorders had truly massive losses in gray matter, particularly in the frontal and prefrontal cortex – two areas that are also hit the earliest and hardest by aging. In patients with long-standing Dysthymic and Bipolar disorder, the loss in hippocampal gray matter volume approached 50%, and is strongly correlated with the number of days of depression the patients experience, as can be seen in Figure 14!72
These findings triggered additional investigation in laboratory animal models of depression, as well as in human patients, and it was at that point that another startling discovery was made: antidepressant drugs, from lithium through the tricyclics, and including the SRRIs, cause brain cells to increase their connectivity and volume. In patients who respond well to these drugs, a significant amount of the gray matter volume loss was reversed. It should also be pointed out that there is brain cell loss in depressive disorders as well, and this is not reversed by drug therapy.73
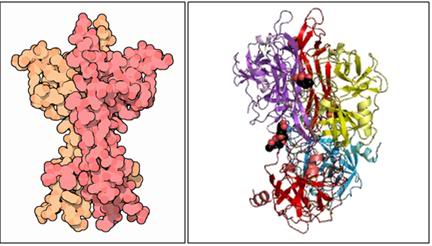 Figure 15: Brain Derived Neurotrophic Growth Factor: space-filling model (left) and ribbon diagram, at right.
Figure 15: Brain Derived Neurotrophic Growth Factor: space-filling model (left) and ribbon diagram, at right.
The logical next question was, “How are these structurally diverse drugs, with very different effects on brain neurotransmission chemistry, acting to stimulate dendritic growth and interneuronal connections?” The answer seems to be that these very molecularly and pharmacologically distinct drugs all activate a brain cell signaling receptor called Tyrosine kinase B (TrkB). In turn, TrkB receptor activation leads to increased expression/secretion of brain-derived neurotrophic factor (BDNF).74,75 And if you are wondering where I am going with this, the answer is that BDNF and related cytokines that are responsible for maintaining neuronal health and neuronal proliferation decline dramatically with age in humans and show a correlation with cognitive impairments, such as memory loss and decreased problem solving ability. In rats, BDNF promotes the growth and proliferation of cells in the hippocampus (both neurons and glial cells) and it is important in long-term potentiation (LTP) and memory formation. Finally, that old standby from the 1940s for treating refractory depression, Electro-Convulsive Therapy (ECT),76 also appears to work, at least in part, by increasing BDNF and related neuroproliferative cytokines.77
BDNF is not alone in maintaining the health of neurons. It is but one of a group of small proteins, a beta polypeptide that belong to a family of nerve growth factors classified as the neurotrophins: Nerve Growth Factor, (NGF), Neurotrophin-3 (NT-3), and Neurotrophin 4/5 (NT-4/5) all of which are essential to the health and survival of cerebrocortical neurons. NGF is essential to the survival and dendritic branching of both central and peripheral neurons; and both types of neurons undergo apoptosis in its absence.78 NGF binds to the high-affinity tyrosine kinase receptor (TrkA), phosphorylating it, which in turn leads to the activation of the PI 3 Kinase, ras, and PLC signaling pathways: all of which are pivotal for maintaining neuronal function and viability. There is even evidence that NGF has systemic effects, and may be responsible for maintaining integrated function of the organism as a whole.79
NGF, the first neurotrophin discovered, was identified in 1951 by Levi-Montalcini and Hamburger80 (although this discovery was disbelieved for well over a decade and NGF was not structurally characterized until the early 1970s.)81,82
By the mid-1980s, NGF was shown to be present in the CSF and brain in adulthood, and to be secreted by neurons in both the hippocampus and the neocortex. This discovery raised the possibility that NGF continued to play a role in the adult Central Nervous System (CNS)83 and in 1986 Hefti et al., reported that injections of NGF into the brains of adult rats prevented the degeneration and death of pre-frontal cortex neurons after axotomy; and shortly thereafter it was demonstrated that NGF reversed the atrophy of pre-frontal cortex neurons and ameliorated deficits in learning and memory in aged rats.84 These neurosalvaging, and possibly even neuroproliferative, effects of NGF, were reduplicated in the brains of Rhesus monkeys, where NGF infusions were demonstrated to rescue lesion-induced cholinergic degeneration.85,86 In 1983, the human NGF receptor was cloned,87 and by the early 1990s infusions of human NGF were reported to prevent degeneration of pre-frontal cortex neurons in non-human primates.88 Of course, the catch proved to be that NGF must be present in the right concentration, at the right place, and at the right time, to be both effective and safe.89
ALZHEIMER’S DISEASE: IMPLICATIONS FOR NORMAL BRAIN AGING
While Alzheimer’s disease (AD) is a distinctly pathological process apart from so called normal brain aging, it may nevertheless spur the development of treatments that may slow, or even reverse, some of the structural and cognitive declines that occur in the cerebral atrophy of ‘healthy’ aging. Interestingly, people with depressive disorders (who also have decreased levels of neurotrophins) have about two times the risk of developing AD.90 Although the precise pathogenesis of AD is unknown, certain abnormal histological features accompany the disease. These pathological features include the accumulation of extracellular amyloid, the formation of intraneuronal neurofibrillary tangles, synapse loss, and cellular degeneration.
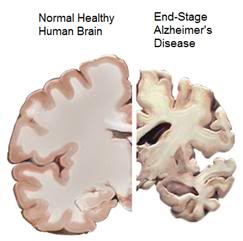 Figure 16: The ravages of End-Stage AD, as shown at right, can be expected to leave little of the brain structure that comprised the individual’s personal identity.
Figure 16: The ravages of End-Stage AD, as shown at right, can be expected to leave little of the brain structure that comprised the individual’s personal identity.
Cellular degeneration in AD occurs in several neuronal populations in the central nervous system. Among the neuronal populations that are most affected, the loss of basal forebrain cholinergic neurons is particularly severe. Loss of cholinergic neurons in AD correlates with severity of dementia, the density of amyloid plaques in the brain, and the amount of synapse loss. To date, the only FDA-approved therapies for AD focus on augmenting the function of degenerating cholinergic
neurons by increasing their production of acetylcholine, or slowing its degradation after secretion. The cholinesterase inhibitor donepezil (Aricept) was the prototypical drug in this class.
Preliminary clinical trials that focused on delivering either NGF or BDNF to the brains of Alzheimer’s patients, via delivery systems implanted into the ventricles of their brains, have shown great promise: in some cases slowing or even arresting progression of the disease.91,92
However, the delivery of these neurotrophins, and in particular NGF, was shotgun, and this lack of targeting resulted in unacceptable adverse effects. The choroid plexus within the cerebral ventricles is the source of the cerebrospinal fluid that bathes and supports the brain and spinal cord. Administration of NGF into the ventricles meant that not only was the entire brain being exposed to the molecule; so were the spinal cord and, ultimately, the larger nerve branches of the peripheral nervous system.93 Patients receiving NGF in this fashion developed severe back pain that was thought to result from NGF reaching nociceptive NGF-responsive cell bodies in the dorsal horns and dorsal root ganglia of the spinal cord, as well as sympathetic axon sprouting around cerebral vasculature,94 and migration and expansion of Schwann cells into a thick cellular layer surrounding the medulla of the brain and the spinal cord.95 These patients also experienced inappetance, with marked and dramatic weight loss, probably as a consequence of NGF-mediated activation of satiety centers in the hypothalamus — a phenomenon that is also seen in rats treated in the same fashion with NGF.96
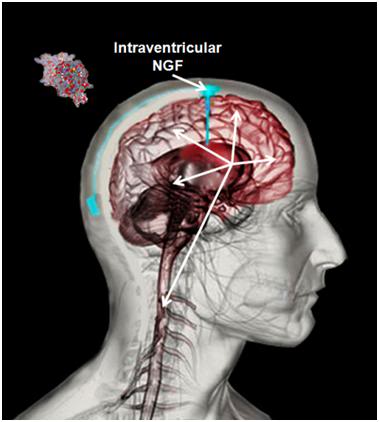 Figure 17: Intraventricular administration of NGF resulted in widespread distribution of the molecule through the central nervous system. This in turn resulted in unacceptable side effects including severe back pain and proliferation of myelin-forming cells.
Figure 17: Intraventricular administration of NGF resulted in widespread distribution of the molecule through the central nervous system. This in turn resulted in unacceptable side effects including severe back pain and proliferation of myelin-forming cells.
So far, gene therapy has been very disappointing in the treatment of disease in humans. I believe that this is about to change and change dramatically in the case of AD. And the need could not be more urgent, because not only are we facing an unprecedented number of AD cases as the baby-boomers enter senescence, drug trials for AD have proven, without exception, complete failures.97-99 As I write this, a number of sophisticated clinical trials employing genetically modified fibroblasts (cultured from and then returned to the patient who is to receive the treatment) are underway. These trials aim to halt cholinergic neuronal degeneration and augment the function of remaining cholinergic neurons by directly elevating choline acetyltransferase (ChAT) function in neurons. These two therapeutic interventions are being achieved via the delivery of human NGF to the brain using genetically engineered cells.
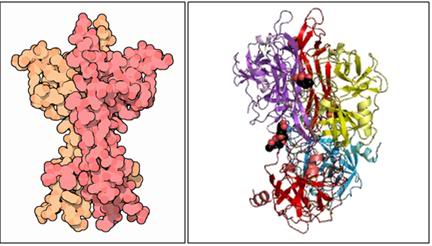 Figure 18: Nerve Growth Factor: space-filling model (left) and ribbon diagram, at right.
Figure 18: Nerve Growth Factor: space-filling model (left) and ribbon diagram, at right.
NGF has been shown to prevent both lesion-induced and spontaneous, age-related degeneration of basal forebrain cholinergic neurons and, even more importantly, NGF infusions reversed both lesion-induced memory loss and spontaneous, age-related memory loss in rodents.100-103
Grafts of primary fibroblasts transduced to express human nerve growth factor have been shown to sustain NGF in vivo gene expression for at least eighteen months in the rodent central nervous system, and these grafts sustain NGF messenger RNA production for at least 14 months in vivo.103 In Rhesus monkeys, ex vivo NGF gene therapy has been demonstrated to sustain NGF protein production in the brain for over a year.[3] In animals from rodents to primates, this procedure has been demonstrated to be safe and well tolerated.104,105
In 2008 an 18 month, open label, prospective Phase I clinical trial of ex vivo gene therapy using the technology developed by Ceregene, Inc., as a treatment for AD patients with a mild degree of cognitive impairment was completed. Participants in the study first underwent skin biopsy to obtain cells for the culture of primary, autologous fibroblasts, which were then genetically modified using an AAV serotype 2-based vector[4] expressing human NGF (CERE-110 ). The patients then underwent carefully targeted intracerebral injections of their own primary fibroblasts delivered to the nucleus basalis of Meynert by stereotactic injection into the region.106,107 This area of the basal forebrain is rich in the cholinergic neurons that are undergoing atrophy and apoptosis as a result of AD. Based upon the positive results from this study, a Phase II randomized, controlled study was initiated by Ceregene in April 2009 (ClinicalTrials.gov identifier: NCT00876863), to evaluate CERE-110 in subjects with mild to moderate AD. The full study results have not yet published; however, the preliminary evidence indicates that the results were positive, with some patients showing marked regression of symptoms and significant cognitive improvement. This was also the case with an earlier study using short-lived fibroblasts.
As is the case in humans, monkeys also experience cerebral atrophy as a consequence of aging. In aged Rhesus monkeys there is atrophy (but not death) of ~40% of basal forebrain cholinergic (BFC) neurons in aging, and ex vivo NGF delivery via genetically modified fibroblasts restored the number of healthy cholinergic neurons to values within 7% of those observed in young monkeys.107 Subsequent experiments in aged primates has also demonstrated that ex vivo gene therapy reversed spontaneous atrophy of BFC neurons.108,109 and reversed cholinergic terminal degeneration through the cerebral hemispheres and midbrain.110,111 Similarly, NGF delivery via ex vivo gene therapy in the aged primate brain also completely restored cholinergic axon density to values observed in young monkeys, and did so without causing any adverse effects. A reason for even greater optimism about the therapeutic promise and long-term utility of this technique is the fact that fibroblasts grafted into the aged primate brain sustained NGF gene expression for at least 18 months, during which time there was marked improvement of both the social and cognitive performance of the animals.112,113
REGULATING NEUROTROPHIN SECRETION
Of course, one problem with engrafting fibroblasts to deliver NGF, or other neurotrophic cytokines, is that they will, necessarily, not be ‘smart’ about when to turn on and off their production of the molecule, and as we have seen in the case of shotgun distribution of NGF in humans, stimulating nerve and glial cell proliferation indiscriminately can have serious adverse effects. Under normal conditions the production of neurotrophic factors is undoubtedly regulated by a feedback loop which prevents both over- and under-secretion of the molecules. It would seem impossible to replicate such a feedback-driven control system absent fully mature genetic engineering technology, but this is not the case. One way it is possible to exercise ‘remote control’ over the implanted fibroblasts, is to genetically engineer them to stop production of the neurotrophin they have been programmed to produce, when minute quantities of a harmless chemical are introduced into their environment.
One system for achieving this end is the ‘tet-off’ viral vector system, which uses tetracycline, or its cousin, doxycycline, to turn on and off neurotrophin production: so called tetracycline regulatable systems.115 The tet-off system has been incorporated into fibroblasts expressing human NGF. Administration of tetracycline in both in vitro and in vivo experiments has demonstrated that NGF production can be regulated by amounts of doxycycline[5] as low as 1 ng/ml, and that NGF gene expression can be suppressed nearly completely within 24 hours of the start of doxycycline administration.116,117 This has allowed for precision control of NGF-dependent neuronal rescue and axonal sprouting in vivo in rats. Similarly, rescue of cholinergic neurons after development of fimbria-fornix lesions was only evident in rats with NGF-expressing grafts that received no doxycycline in their drinking water, or in other words, only when NGF expression was activated. Animals that received doxycycline (NGF expression turned “off”) failed to show cholinergic neuronal protection after lesioning of the fimbria-fornix.117 Thus, it is now possible to exercise exquisite and rapid control of NGF expression in the mammalian brain by using a tet-off control vector system.
End of Part 2
Footnotes
[1] This same phenomenon is also strikingly present in most patients with Alzheimer’s disease and other cognition eroding dementias. The overwhelming majority of such patients refuse to acknowledge that they are experiencing cognitive cuts even when this is confirmed by several individuals with whom they enjoy a good relationship.
[2] Yet another indication that, as Aschwin de Wolf has pointed out, “Gerontology is too important to leave to the gerontologists,” just as Cryobiology has proved too important to leave to the cryobiologists. We’ll have to do our own work to save our own lives.
[3] MH Tuszynski, the lead investigator in the initial Rhesus monkey studies recently stated during a television interview that they have now demonstrated survival of engrafted fibroblasts with retention of NGF secretion out to 5 years.
[4] Adeno-associated virus vectors (AAV) are genetically engineered versions of the human adenovirus – a virus that causes a common cold- like illness in people.
[5] Doxycycline is used as the controlling molecule as opposed to tetracycline because it more readily crosses the blood brain barrier and also has greater penetration into the myelinated axons of the peripheral nervous systems. The dose of tetracycline needed to operate the tet-off system is so low that it has no other therapeutic effect and is below the threshold required for antimicrobial activity.
References
55) Yassa, MA, Tugan, T, Muftuler, L, Starka, CEL. Ultrahigh-resolution microstructural diffusion tensor imaging reveals perforant path degradation in aged humans in vivo. PNAS. 2010;107:12687–12691.
56) Bucur, B, Madden, DJ, Spaniol, J, Provenzale, JM, Cabeza, R, White, LE, Huettel, SA. Age-related slowing of memory retrieval: contributions of perceptual speed and cerebral white matter integrity. Neurobiol Aging. 2008;29:1070–1079.
57) Schaie, K. W. Intellectual Development in Adulthood: The Seattle Longitudinal Study. Cambridge Univ. Press, 1996.
58) Gunning-Dixon, FM, Head, D, McQuain, J, Acker, JD, Raz, N. Differential aging of the human striatum: a prospective MR imaging study. AJNR Am J Neuroradiol. 1998;(8):1501-7.
59) Schaie, K. W. Intellectual Development in Adulthood: The Seattle Longitudinal Study. Cambridge Univ. Press, Cambridge, 1996.
60) Grady, CL, Maisog, JM, Horwitz, B, Ungerleider, LG, Mentis, MJ, Salerno, JA, Pietrini, P, Wagner, E, Haxby, JV. Age-related changes in cortical blood flow activation during visual processing of faces and location. J Neurosci. 1994;14:1450–1462.
61) Madden, DJ, Connelly, SL, Pierce, TW. Adult age differences in shifting focused attention. Psychol Aging. 1994;9:528-538.
62) Cabeza, R, Daselaar SM, Dolcos F, Prince SE, Budde M, Nyberg L. 2004. Task-independent and task-specific age effects on brain activity during working memory, visual attention and episodic retrieval. Cereb Cortex. 14:364–375.
63) Grady, CL, McIntosh, AR, Craik, FI. Task-related activity in prefrontal cortex and its relation to recognition memory performance in young and old adults. Neuropsychologia. 2005;43:1466–1481.
64) Schneider, B, Pichora-Fuller, MK. Implications of perceptual deterioration for cognitive aging Research. In: Craik, FI, Salthouse, TA, editors. The handbook of aging and cognition, Psychology Press, 2000. ISBN-10: 080585990X
65) Lindenberger U, Baltes PB. Sensory functioning and intelligence in old age: a strong connection. Psychol Aging. 1994;9:339-355.
66) Williamson, RN, Gunning-Dixon, A, Head, F, Acker, JD. Neuroanatomical and cognitive correlates of adult age differences in acquisition of a perceptual-motor skill. Microsc Res Tech. 2000;51(1):85-93.
67) Jang, SW, Liu, X, Chan, CB, Weinshenker, D, Hall, RA, Xiao, G, Ye, K. Amitriptyline is a TrkA and TrkB receptor agonist that promotes TrkA/TrkB heterdodimerization and has potent neurotrophic activity. Chemistry and Biology. 2009;16, x-y.
68) Kelwala, S, Stanley, M, Gershon, S. History of antidepressants: successes and failures. J Clin Psychiatry. 1983;44(5 Pt 2):40-8.
69) Nutt, DJ, Forshall, S, Bell, C, Rich, A, Sandford, J, Nash, J, Argyropoulos, S. Mechanisms of action of selective serotonin reuptake inhibitors in the treatment of psychiatric disorders. European Neuropsychopharmacology. 1999:9, Supp3, S81-S86.
70) Martinowich, K, Lu, B. Interaction between BDNF and Serotonin: Role in Mood Disorders. Neuropsychopharmacology. 2008;33:73–83.
71) Bostwick, JM, Pankratz, VS. Affective Disorders and Suicide Risk: A Reexamination. Am J Psychiatry. 2000;157:1925-1932.
72) Rantamäki ,T, Hendolin, P, Kankaanpää, A, Mijatovic, J, Piepponen, P, Domenici ,E, Chao, MV, Männistö, PT, Castrén ,E. Pharmacologically diverse antidepressants rapidly activate brain-derived neurotrophic factor receptor TrkB and induce phospholipase-Cgamma signaling pathways in mouse brain. Neuropsychopharmacology. 2007 Oct 32 (10):2152-62. Epub 2007 Feb 21. PMID: 17314919.
73) Saarelainen, T, Hendolin, P, Lucas, G, Koponen, E, Sairanen ,M, MacDonald, E, Agerman, K, Haapasalo, A, Nawa, H, Aloyz, R, Ernfors, P, Castrén, E. Activation of the TrkB neurotrophin receptor is induced by antidepressant drugs and is required for antidepressant-induced behavioral effects. J Neurosci. 2003 Jan 1 ;23(1):349-57. PMID: 12514234.
74) Sairanen, M, Lucas, G, Ernfors, P, Castrén, M, Castrén, E. Brain-derived neurotrophic factor and antidepressant drugs have different but coordinated effects on neuronal turnover, proliferation, and survival in the adult dentate gyrus. J Neurosci. 200;25(5):1089-94. PMID: 15689544.
75) Sheline, YI, Wang, PW, Gado, MH, Csernansky, JG, Vanier, MW. Hippocampal atrophy in recurrent major depression. Proc. Natl Acad Sci Medical Sciences 1996;93:3908-3913.
76) Groves, JO. Is it time to reassess the BDNF hypothesis of depression? Mol Psychiatry 2007;12: 1079–1088.
77) Mughal, MR, Baharani, A, Chigurupati, S, Son, TG, Chen, E, Yang, P, Okun, E, Arumugam,T, Chan, SL, Mattson, MP. Electroconvulsive shock ameliorates disease processes and extends survival in Huntington mutant mice. Hum Mol Genet. 2010;Dec 3. [Epub ahead of print] PMID: 21106706.
78) Freeman, RS, Burch, RL, Crowder, RJ, Lomb, DJ, Schoell, MC, Straub, JA, Xie, L. NGF deprivation-induced gene expression: after ten years, where do we stand? Prog Brain Res. 2004;146: 111–26. PMID 14699960.
79) Levi-Montalcini, R. The nerve growth factor and the neuroscience chess board. Prog. Brain Res. 2004;146: 525–7. PMID 14699984.
80) Levi-Montalcini, R, Hamburger, V: Selective growth stimulating effects of mouse sarcoma on the sensory and sympathetic nervous system of the chick embryo. J Exp Zool. 1951;116:321-362.
81) Angeletti, RH, Bradshaw, RA, Wade, RD: Subunit structure and amino acid composition of mouse submaxillary gland nerve growth factor. Biochemistry. 1971;10:463-469.
82) Bocchini V, Angeletti PU: The nerve growth factor: purification as a 30,000-molecular-weight protein. Proc Natl Acad Sci USA. 1969; 64:787-794.
83) Korsching, S, Auburger, G, Heumann, R, et al: Levels of nerve growth factor and its mRNA in the central nervous system of the rat correlate with cholinergic innervation. J. EMBO. 1984;4:1389-1393.
84) Hefti ,F: Nerve growth factor promotes survival of septal cholinergic neurons after fimbrial transections. J Neurosci. 1986;6:2155-2162.
85) Fischer, W, Wictorin, K, Bjorklund, A, et al. Amelioration of cholinergic neuron atrophy and spatial memory impairment in aged rats by nerve growth factor. Nature. 1987;329:65-68.
86) Koliatsos, VE, Nauta, HJ, Clatterbuck, RE, et al. Mouse nerve growth factor prevents degeneration of axotomized basal fore-brain cholinergic neurons in the monkey. J Neurosci. 1990;10:3801-3813.
87) Fischer, W, Wictorin, K, Bjorklund, A, et al: Amelioration of cholinergic neuron atrophy and spatial memory impairment in aged rats by nerve growth factor. Nature. 1987;329:65-68.
88) Koliatsos ,VE, Nauta, HJ, Clatterbuck, RE, et al: Mouse nerve growth factor prevents degeneration of axotomized basal fore-brain cholinergic neurons in the monkey. J Neurosci. 1990;10: 3801-3813.
89) Tuszynski, MH, U, HS, Amaral, DG, et al. Nerve growth factor infusion in the primate brain reduces lesion-induced cholinergic neuronal degeneration. J Neurosci. 1990; 10:3604-3614.
90) Saczynski, JS, Beiser, A, Seshadri, S. Auerbach, S, Wolf, PA, Au, R. Depressive symptoms and risk of dementia: The Framingham Heart Study. Neurology. 2010;75:35.
91) Seiger, A, Nordberg, A, von Holst, H, Bäckman, L, Ebendal, T, Alafuzoffm, I, Amberla, K, Hartvig, P, Herlitz, A, Lilja, A, et al. Intracranial infusion of purified nerve growth factor to an Alzheimer patient: the first attempt of a possible future treatment strategy. Behav Brain Res. 1993;57(2):255-61. PubMed PMID:8117429.
92) Eriksdotter, Jönhagen, M, Nordberg, A, Amberla, K, Bäckman, L, Ebendal, T, Meyerson, B, Olson, L, Seiger, Shigeta, M, Theodorsson ,E, Viitanen, M, Winblad, B, Wahlund, LO. Intracerebroventricular infusion of nerve growth factor in three patients with Alzheimer’s disease. Dement Geriatr Cogn Disord. 1998;9(5):246-57. PMID: 9701676.
93) Emmett, CJ, Stewart, GR, Johnson, RM, et al: Distribution of radioiodinated recombinant human nerve growth factor in primate brain following intracerebroventricular infusion. Exp Neurol. 1996;140:151-160.
94) Eriksdotter-Jonhagen M, Nordberg, A, Amberla, K, et al: Intracerebroventricular infusion of nerve growth factor in three patients with Alzheimer s disease. Dement Geriatr Cogn Disord. 1998;9:246-257.
95) Winkler, J, Ramirez, GA, Kuhn, HG, et al: Reversible Schwann cell hyperplasia and sprouting of sensory and sympathetic neurites in vivo after intraventricular administration of nerve growth factor. Ann Neurol. 1997;41:82-93.
96) Cordeira, JW, Frank, L, Sena-Esteves, M, Pothos, EN, Rios, M. Brain-derived neurotrophic factor regulates hedonic feeding by acting on the mesolimbic dopamine system. J Neurosci. 2010 Feb 17;30(7):2533-41.
97) Smith, AD. Why are drug trials in Alzheimer’s disease failing? Lancet. 2010 Oct 30;376(9751):1466. PubMed PMID: 21036274.
98) Extance, A. Alzheimer’s failure raises questions about disease-modifying strategies. Nat Rev Drug Discov. 2010;(10):749-51. PMID: 20885394.
99) (Disease-modifying drug fails in Alzheimer’s study. Harv Ment Health Lett. 2010;(10):7. PubMed PMID: 20503478.
100) Francia, N, Cirulli, F, Chiarotti, F, Antonelli, A, Aloe, L, Alleva, E. Spatial memory deficits in middle-aged mice correlate with lower exploratory activity and a subordinate status: role of hippocampal neurotrophins. Eur J Neurosci. 2006;(3):711-28. PMID: 16487153.
101) Hwang. IK, Yoo, KY, Jung, BK, Cho, JH, Kim, DH, Kang, TC, Kwon, YG, Kim, YS, Won MH. Correlations between neuronal loss, decrease of memory, and decrease expression of brain-derived neurotrophic factor in the gerbil hippocampus during normal aging. Exp Neurol. 2006;201(1):75-83. Epub 2006 May 5. PMID: 16678162.
102) Pertusa, M, García-Matas, S, Mammeri, H, Adell, A, Rodrigo, T, Mallet, J, Cristòfol, R, Sarkis, C, Sanfeliu, C. Expression of GDNF transgene in astrocytes improves cognitive deficits in aged rats. Neurobiol Aging. 2008;(9):1366-79. Epub 2007 Mar 30. PMID: 17399854.
103) Conner, JM, Darracq, MA, Roberts, J, Tuszynski, MH. Nontropic actions of neurotrophins: subcortical nerve growth factor gene delivery reverses age-related degeneration of primate cortical cholinergic innervation. Proc Natl Acad Sci U S A. 2001;98(4):1941-6.
104) Smith, DE, Roberts, J, Gage, FH, Tuszynski, MH. Age-associated neuronal atrophy occurs in the primate brain and is reversible by growth factor gene therapy. Proc Natl Acad Sci U S A. 1999;96(19):10893-8.
105) Klein, RL, Hirko, AC, Meyers, CA, Grimes, JR, Muzyczka, N, Meyer, EM. NGF gene transfer to intrinsic basal forebrain neurons increases cholinergic cell size and protects from age-related, spatial memory deficits in middle-aged rats. Brain Res. 2000;875(1-2):144-51. PMID: 10967308.
106) http://www.redorbit.com/news/video/health/4/gene_therapy_for_alzheimers_disease/22520/ . Retrieved 17 December, 2010.
107) (Mandel, RJ. CERE-110, an adeno-associated virus-based gene delivery vector expressing human nerve growth factor for the treatment of Alzheimer’s disease. Curr Opin Mol Ther. 2010;(2):240-7. PMID: 20373268.
108) Schulte-Herbrüggen. O, Jockers-Scherübl, MC, Hellweg R. Neurotrophins: from pathophysiology to treatment in Alzheimer’s disease. Curr Alzheimer Res. 2008;(1):38-44. Review. PMID: 18288930.)
109) Kordower, JH, Winn SR, Liu, YT, et al. The aged monkey basal forebrain: rescue and sprouting of axotomized basal fore-brain neurons after grafts of encapsulated cells secreting human nerve growth factor. Proc Natl Acad Sci USA. 1991;91:10898-10902. http://www.redorbit.com/news/video/health/4/gene_therapy_for_alzheimers_disease/22520/ Retrieved 17 December, 2011.
110) Conner, JM, Darracq, MA, Roberts, J, Tuszynski, MH. Nontropic actions of neurotrophins: subcortical nerve growth factor gene delivery reverses age-related degeneration of primate cortical cholinergic innervation. Proc Natl Acad Sci U S A. 2001;98(4):1941-6.
111) Kordower, JH, Winn, SR, Liu, YT, et al: The aged monkey basal forebrain: rescue and sprouting of axotomized basal fore-brain neurons after grafts of encapsulated cells secreting human nerve growth factor. Proc Natl Acad Sci USA. 1991;91:10898-10902. http://www.redorbit.com/news/video/health/4/gene_therapy_for_alzheimers_disease/22520/ . Retrieved 17 December, 2010.
112) Smith, DE, Roberts J, Gage, FH, et al: Age-associated neuronal atrophy occurs in the primate brain and is reversible by growth factor gene therapy. Proc Nat Acad Sci USA. 1999;96:10893-10898.
113) Koliatsos, VE, Clatterbuck, RE, Nauta, HJ, et al: Human nerve growth factor prevents degeneration of basal forebrain cholinergic neurons in primates. Ann Neurol. 1991;30:831-840.)
114) Tuszynski, MH, Sang, H, Yoshida, K, et al. Recombinant human nerve growth factor infusions prevent cholinergic neuronal degeneration in the adult primate brain. Ann Neuro.l 1991;30:625-636.
115) Gossen, M, Bonin, AL, Freundlieb, S, et al. Inducible gene expression systems for higher eukaryotic cells. Curr Opin Biotechnol. 1994;5:516-520.
116) Blesch, A, Conner, JM, Tuszynski, MH: Modulation of neuronal survival and axonal growth in vivo by tetracycline-regulated neurotrophin expression. Gene Ther. 2001;8:954-960.
117) Blesch, A, Uy, HS, Diergardt, N, et al. Neurite outgrowth can be modulated in vitro using a tetracycline-repressible gene therapy vector expressing human nerve growth factor. J Neurosci Res. 2000;59:402-409.
