By Mike Darwin
THE PROBLEM OF NO FEEDBACK
How did these things happen? How did sincere, hard working, committed people who desperately wanted cryonics for themselves allow the situations I’ve just described – the woefully inadequate perfusion capabilities (or more properly, lack thereof) and the madness of racking patients head-up in their storage dewars?
And what about Dr. Bedford? How was it possible for his care to have been so botched while the media, and the overwhelming majority of cryonicists, remained convinced that he had been cryopreserved under seemingly good conditions?
Even more incredibly, let‘s stop and reconsider Chatsworth with greater care. Yes, Robert Nelson was a fraud and sociopath – no question about that.
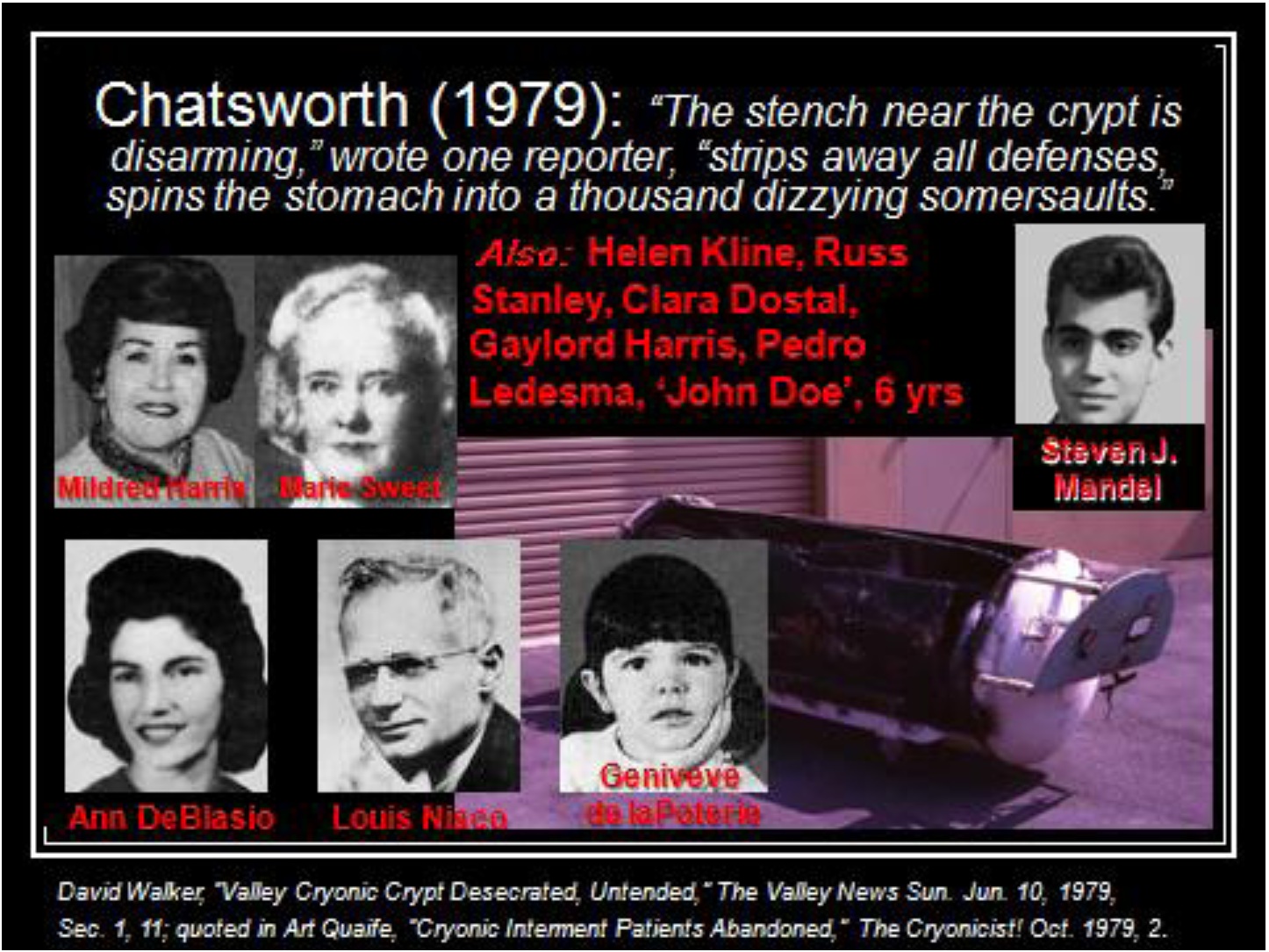
But the rest of CSC‘s membership was neither sociopathic nor fraudulent. They were very sincere and deeply committed cryonicists. Marie Sweet, Helen Kline, Russ Stanley, and the father of 8 year old Genivieve de la Poteri, were all CSC members who were involved with the organization for months or years before they themselves were cryopreserved and ended up as skeletal remains at Chatsworth.
Virtually all of the other CSC members were decent people. Several of them had put tens of thousands of (1968-9) dollars of their savings into the CSC facility. All of these people refused to believe that anything was amiss at the Chatsworth facility until the press broke the story in 1979! On average CSC members were intelligent professionals, entrepreneurs, small business people and, above all, independent thinkers. How was it possible that, even as evidence accumulated that “things just didn‘t add up” with CSC‘s storage operation, they continued to have confidence in CSC?
In fact, of the 30 or so “signed up” CSC members at the time, only two became suspicious, investigated, and left the organization; Fred and Linda Chamberlain. And in the cryonics community at large, only three people were likewise deeply suspicious (or virtually certain) that something was amiss with CSC: Curtis Henderson, Saul Kent and me.
In 1986 I wrote an article entitled the “Myth of the Golden Scalpel” which first delineated the problem of “no feedback” in cryonics. The article was a response to intense criticism of the application of an evidence based, medical model to cryonics and the associated increase in costs and, perhaps just as importantly, the accompanying disempowerment of “amateurs.” Prior to the entry of professionals – or people working to create professionalism in cryonics – cryonics was a “do it yourself” (DIY) undertaking and anybody could (and did) undertake to cryopreserve people. A corollary of this was that anyone‘s opinions about how cryonics should be practiced were as good and as valued as anyone else‘s. Much of this criticism came from members of the Bay Area Cryonics Society (BACS) and the Cryonics Institute (CI).
In the next part of this lecture, I will show you images of the cryoprotective perfusion of a CSNY patient from 1972. That is very close to how CI carried out their perfusions at that time, and indeed, it was not until Ben Best arrived at CI that even the simplest and most basic parameters of patient care were monitored or recorded. And even now, CPA perfusion at CI more closely resembles what you will see in the slides from 1972 than it does what you will see still later when the Chamberlains, Jerry Leaf and I began changing cryonics.
The kind of procedures being used before the application of an evidence based medical model to cryonics are best described as ritual, not science. There were no truly meaningful tests, measurements or evaluations performed to inform the people carrying out cryopreservation procedures whether things went poorly or well and whether the “standard” procedure (or a modified one) was good or bad for a given patient.
For instance, should patients with long ischemic times get a different treatment than patients with short or very little ischemic times? Perhaps a more rapid increase in CPA concentration should be used, or even no CPA perfusion at all under some circumstances? How and why such decisions are to be made should be documented and have a scientific basis which is continually being informed by ongoing research.
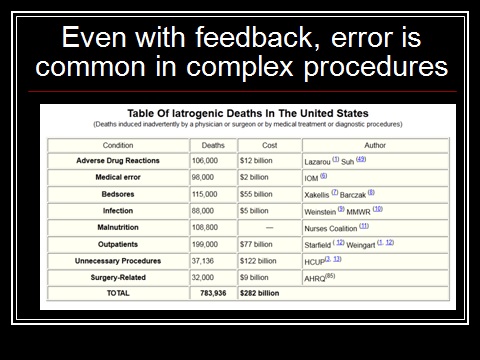
In conventional medicine, where personnel at all levels are extensively trained, those who control the discipline are highly educated and skilled professionals; there is licensing and government oversight, and extensive documentation of procedures and record keeping. Lethal and morbid injuries are surprisingly common. As you can see, in the US alone, there are over three quarters of a million deaths each year due to medical error (iatrogenesis).
This is a staggering number of deaths and the associated cost is an estimated $282 billion! And keep in mind this does not include the patients who are injured and do not die, or the many patients whose death or injury is either not detected, or not reported.
SLIDE 90
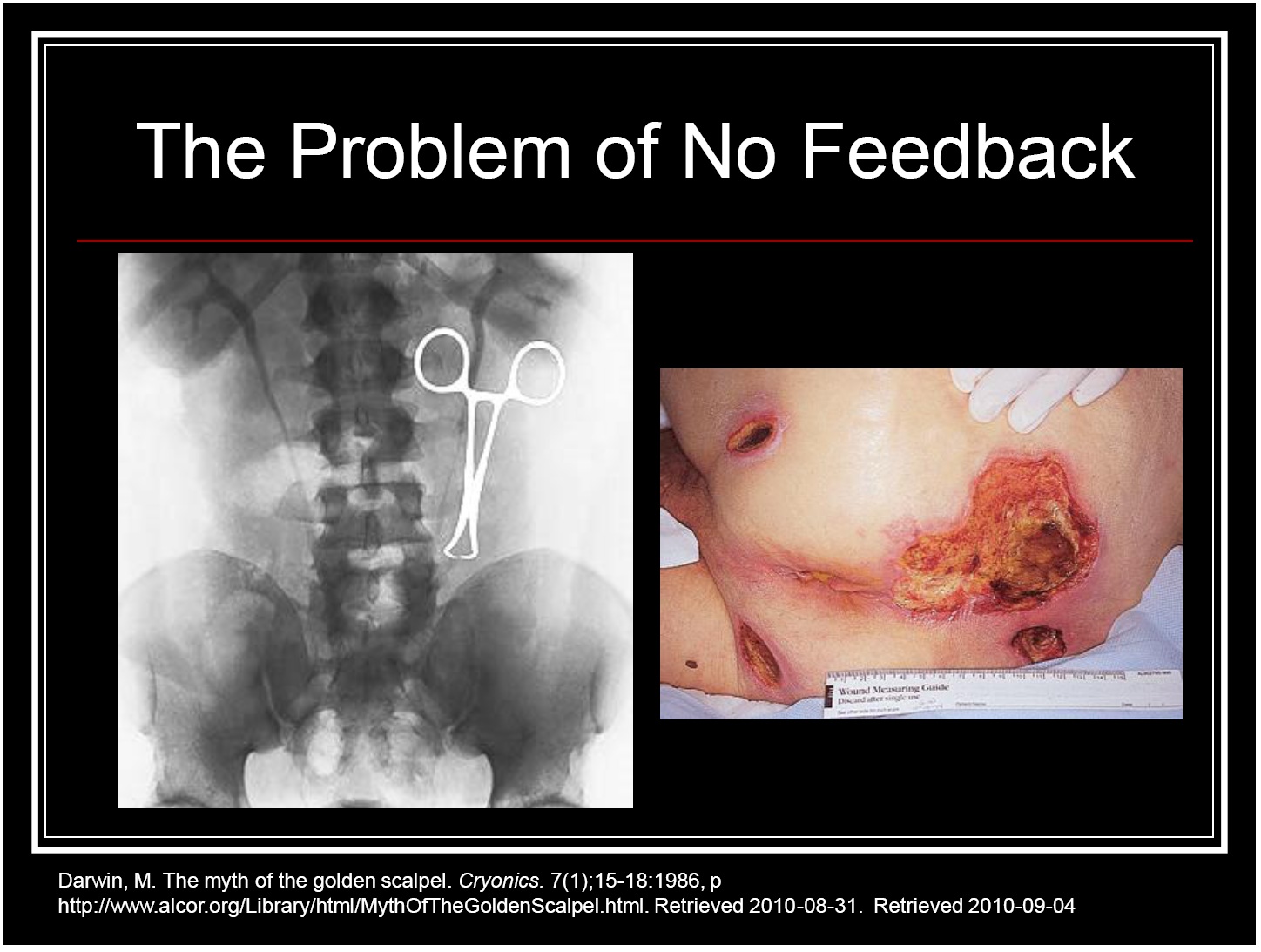
As bad as the problem is, it would be much worse if it were not for the fact that in medicine the patients being treated provide feedback. If you injure a patient delivering medical care, the odds are good that the patient will show both symptoms and signs of your error. He may suffer pain, become gravely ill, behave abnormally, lose sensory or motor function, be disfigured, or die.
The image at the right of this slide is of a decubitus ulcer – a bedsore or pressure sore, in common parlance – due to failure to properly position and turn the patient. Bedsores are surprisingly common because the patient does not feel the discomfort until after the injury at the pressure point(s) has occurred. Patients in extended care facilities are also often effectively “voiceless objects” who are frequently demented and are often unable to speak articulately for themselves even when compos mente. All too often they are also being warehoused and cared for by under-trained or under-motivated personnel.
Medicine also benefits from diagnostic modalities, such as the x-ray image at right, which allows for errors to be uncovered more effectively – and thus be corrected or mitigated – where it‘s possible to do so.
Unfortunately, the cryonics patient can provide none of the feedback a living patient does and as I have often said before, a patient who is straight frozen invariably looks far better and far more lifelike and at peace than a patient who has received the best available care.
LACK OF PROFESSIONALISM
If the cryonics patient was not in a bad enough position as a result of the no feedback problem, the situation becomes even worse when he is being cared for by personnel who have no extensive real-world experience in biomedicine (both in clinical and research environments) IN ADDITION to specialized training to integrate that experience into the context of cryonics as medicine.
Here I would like to use an example which is incredibly frustrating to me because it has recurred, even with people delivering care to cryonics patients who have been told about this problem and given a clear explanation as to how to avoid it.
It‘s a “mechanical” problem that I think is easily understood, so I‘m using it as an example. There are many, many other more complex and subtle problems that would be much more difficult to communicate in the available time.
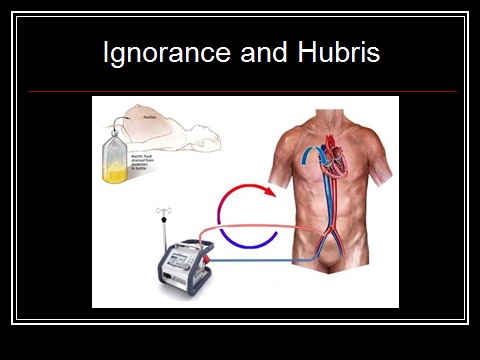
When blood washout and extracorporeal support are performed in the field it is necessary to access the circulatory system by cannulating the femoral artery and vein in the groin. When cardiopulmonary bypass (CPB) is carried out in this fashion the blood flows through the blood vessels in a retrograde fashion – in other words, in the opposite direction from which it normally flows.
Because the blood being pumped from the circuit into the patient is being pumped under pressure into the femoral artery, a short cannula of modest diameter may be used. However, the venous blood, flowing from the body and into the bypass circuit, is flowing at very low pressure, typically at 5-10 mm Hg and its flow into the circuit reservoir is due to gravity.
As a result, a larger diameter cannula which is much longer must be used. Ideally, we would like to position the tip of that cannula at the level of the right heart, where the blue arrow is on this schematic. However, that is not possible to do in the field without x-ray (fluoroscopic) assistance. Thus, the cannula tip is usually in the inferior vena cava somewhere below the level of the diaphragm where the white arrow is pointing. This barely allows for enough venous blood flow out of the patient – even under the best conditions.
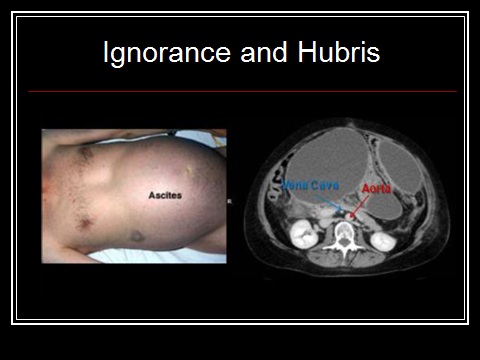
Now, if the patient has a large volume of fluid in his abdomen, a condition called ascites, or is very obese, what happens is that the pressure from all the fluid or fat compresses the very thin and flexible walls of the vena cava and prevents adequate venous return. In fact, it‘s a wonder that any flow can proceed under ‗normal‘ circumstances.
The MRI at right shows a typical ascitic abdomen in cross section. Contrast media has been given intravenously so that the blood vessels show up distinctly. You can see the aorta clearly, but the inferior vena cava, which is normally twice the diameter of the aorta, appears as a small white dot, compressed as it is by the large volume of intra-abdominal fluid.
Ascites is not uncommon in cryonics patients since it occurs in cases of liver failure, cancer which has invaded the liver, congestive heart failure, cirrhosis, ovarian cancer and a number of other conditions. If a cryopatient presents with ascites one of two things must be done before femoral-femoral CPB is undertaken. The ascites may be drained by the simple expedient of making a stab wound through the body wall and placing a drainage tube in the peritoneal cavity, or an alternative venous drainage site must be selected, such as the internal jugular vein.
Failure to do one or the other of these things will result in either no venous return, or inadequate venous return. In the latter case the effect will be the very rapid development of massive system and cerebral edema due to the increased pressure in the venous circulation.
This problem has occurred at least five times in cryonics cases that I know of, and in four of those five cases, it happened to personnel who had experienced the same problem before. And yet, the problem was not addressed and the same rote procedure was followed despite the fact that problems were evident. I will say that in the two cases where there was no venous return they did eventually stop perfusion because they realized that ‗something was wrong.‘
The solutions to this problem are not easy because they demand the acquisition of professionalism, knowledge, and skill in the context of cryonics as medicine. We came very close to doing that in the decade between 1981 and 1991. But we failed. Why we failed I‘ll discuss later. Suffice it to say that the problem of maintaining professionalism is a nettlesome one in medicine, engineering and other demanding disciples, and there will be no quick fixes. In cryonics, where almost all the feedback we get from our patients must be artificially generated, the problem will be much more difficult to solve.
As we’ve already seen, patients can even have completely decomposed – and the cryonics organization can continue to operate, not just for weeks or months, but for years after this has occurred – all the while continuing to accept more patients!
I selected the image for this slide with special care, because it points up one of the many serious problems lack of professionalism in cryonics has caused. Repeatedly in the history of cryonics those in leadership positions within cryonics organizations have hired and placed in positions of power family members, close friends and cronies, with little (and usually no) respect to their qualifications. The most glaring recent example of this was when a former CEO of a cryonics organization hired his wife, his daughter and his son-in-law as paid full and part time staff. Professionalism is anathema to nepotism. Professionalism is first and foremost a meritocracy.
What is cryonics professionalism? The short answer is that it does not yet exist, per se. If and when it does, the short definition is that cryonics professionalism is adherence to a set of values comprising both a formally agreed-upon code of conduct and the informal expectations of colleagues, clients and the cryonics community.
The key values include acting in a patient’s interest, striving to improve the quality and length of a patient‘s pre-cryopreservation life, and maintaining the highest standards of excellence in the practice of cryonics and in the generation and dissemination of knowledge. In addition to scientific, medical, technical knowledge and skills, cryonics professionals should present psychosocial and humane qualities such as caring, empathy, humility and compassion, as well as deep commitment to assisting the individual patient and the community of cryonicists as a whole in their pursuit of indefinitely extended life and health. All these qualities are expected of members of highly trained cryonics professionals. I believe that, at a minimum, these things must be present in the cryonics professional:
Professional Commitment to Patient Welfare constitutes the essence of professionalism and is based on the rule that the best interest of patients and not self-interest is the professional obligation. Professional Accountability is an important element of professionalism which is required of cryonics professionals at several levels: to their patients for fulfilling the implied contract governing the patient/professional relationship, to the cryonics community for addressing their health needs, and to their profession for adhering to cryonics‘ ethical precepts.
Professional Duty can be expressed by the free acceptance of a commitment to service, availability and responsiveness when “on call,” accepting inconvenience to meet the needs of patients, by enduring unavoidable risks to oneself when a patient’s welfare is at stake, and by advocating the best possible care regardless of the patient’s ability to pay. It is a willingness to seek an active role in professional organizations and volunteering ones skills and expertise for the welfare of cryonics as a discipline and a way of life, and of the cryonics community.
Professional Excellence entails a conscientious effort to exceed ordinary expectations. Commitment to excellence is an acknowledged goal for all cryonics professionals and includes a commitment to life-long learning.
Professional Honor and Integrity implies being fair, being truthful, keeping one’s word, meeting commitments, and being straightforward. It also requires recognition of the possibility of conflict of interest and avoiding any situation in which the interest of the cryonics professional is placed above that of the patient or allowing personal gain to supersede the best interest of the patient. This is an integral part of professionalism. The importance of professionalism in the patient/cryonics professional relationship cannot be overstated.
Professional Respect for Others is reflected in the respect towards the patients and their families, other cryonics professionals and professional colleagues such as physicians, nurses, perfusionists, paramedics, and health sciences technicians and therapists. It is the essence of basic, decent conduct and is both central to professionalism and fundamental to enhancing collegiality among cryonics professionals.
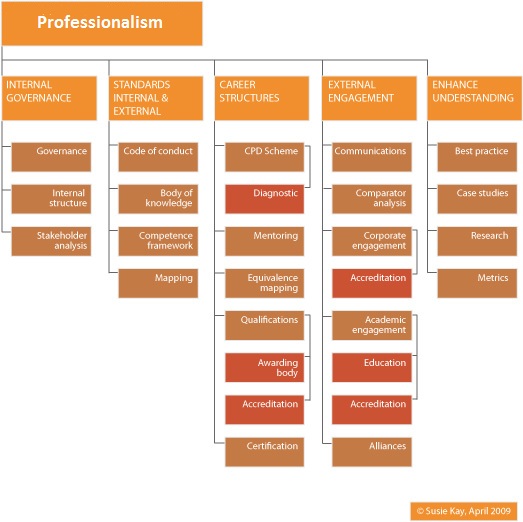
Until a solid professional base is created in cryonics there can be no enduring success. What you see here are the elements of a mature professionalism, in this case in medicine. You will note that at the left that formal (written) standards and practices, a code of conduct and governance for implementing these things, are among the first elements of professionalism.
It is not necessary for cryonics, in its current microscopic and flawed implementation to create all of the elements shown here – nor is it possible. But what we must do is to begin at the beginning and create standards and practices for every element of the program and both follow and enforce them diligently.
End of Initialization Failure, Part 4

> This is a staggering number of deaths and the associated cost is an estimated $282 billion! And keep in mind this does not include the patients who are injured and do not die, or the many patients whose death or injury is either not detected, or not reported.
Following image is broken.
Thanks for bringing this to my attention. The weather is good here (it snowed at few days ago!) and I am doing construction work outside whilst I can. The missing image is of an x-ray showing a Backhaus towel clip accidentally left inside the abdomen of a surgical patient, and of a decubitus ulcer (bedsore) on the sacrum of another patient: both images were obtained from the web and are perfectly pedestrian and in no way lewd or lascivious. However, Photobucket, the image hosting service I use, has extremely strict policies on the kind of images they allow. Whatever filtering mechanism they use is quite quirky about showing unclothed bodies or parts thereof. It is almost impossible to predict what they will censor. I have learned that most Reconnaissance and Classical art will be censored – for instance, the Venus de Milo has a good chance of being censored. I am sending the missing image to the Webmaster of Chronosphere, Eugen Leitl, who can (hopefully) replace it in the text. Eugen has urged me to drop Photobucket and use another hosting service. I’m willing to do this, however Photobucket is is extremely easy to use, very reliable and very inexpensive. Having said that, they are completely “unresponsive” to questions and complaints and deal with clients by using automated, generic responses. — Mike Darwin