How to avoid autopsy and long ‘down-time’
(ischemia) ~85% of the time!
By Mike Darwin
Removing a Central Objection to Cryonics
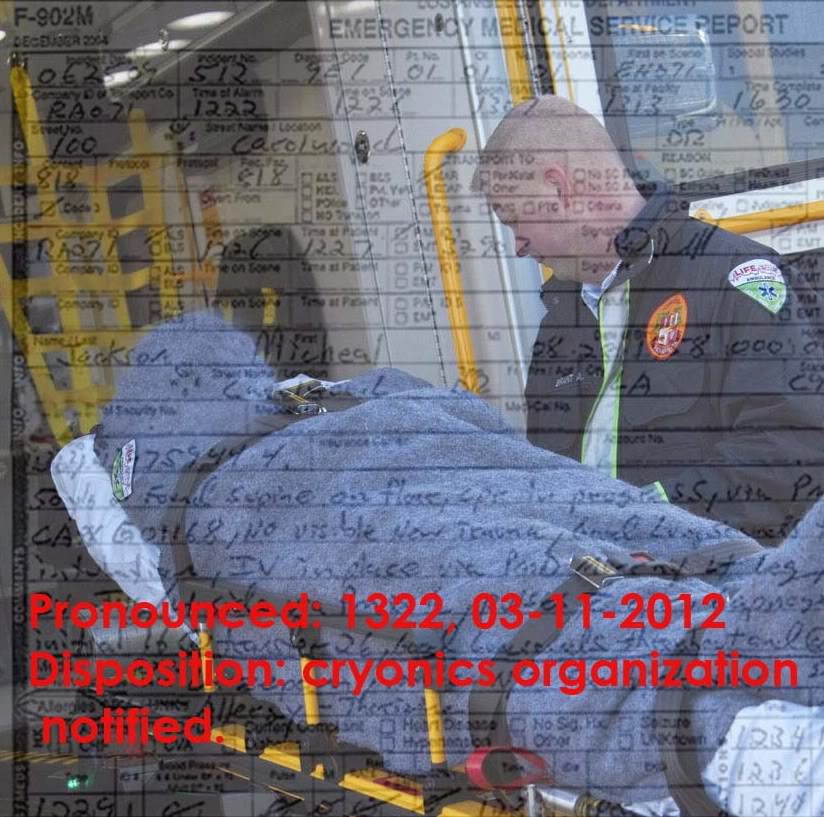
In case you missed it, what I just said in that slim paragraph at the end of the preceding part of this article has profound implication because it has the potential to remove what is unarguably one of the largest and the most rational objections that there are to cryonics. That objection is that roughly two-thirds of those who have made cryonics arrangements will not be cryopreserved under good conditions, and that half of all those signed up will be cryopreserved under very adverse conditions, such as autopsy or long (greater than 12 hours) post cardiac arrest delay. The recent advances in non-invasive medical imaging I’m about to discuss here offer the opportunity to we cryonicists to make many, if not most such losses all but unnecessary.
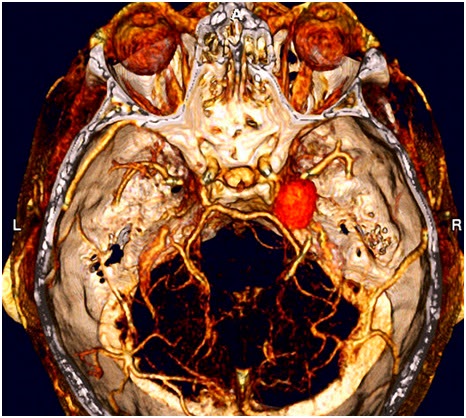 Figure 17: False color CT 3-D reconstruction of a patient’s intracranial arterial vascular tree. The orange-red, cheery shaped anomaly behind the right eye is a large aneurysm. The brain and other intracranial soft tissues have been digitally subtracted to facilitate a complete and unobstructed view of the patient’s arterial vasculature.
Figure 17: False color CT 3-D reconstruction of a patient’s intracranial arterial vascular tree. The orange-red, cheery shaped anomaly behind the right eye is a large aneurysm. The brain and other intracranial soft tissues have been digitally subtracted to facilitate a complete and unobstructed view of the patient’s arterial vasculature.
The image that you see in Figure 17 is now a perfectly pedestrian medical image that can be obtained from a garden variety CT scanner available at most diagnostic imaging centers in mid-sized cities anywhere in the world. This particular image has the brain, the soft tissue and everything digitally subtracted from it but the patient’s arterial tree and skull. The cherry shaped protrusion on the right is an aneurysm which, if were to rupture, could cost the patient his life or leave him profoundly disabled.
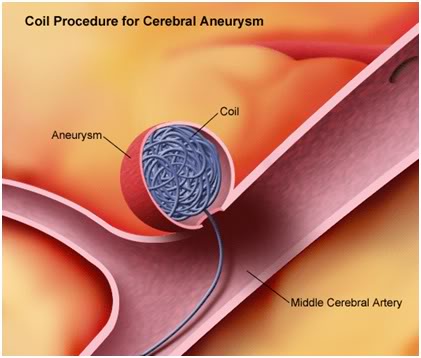
Figure 18: Many brain aneurysms can be treated non-surgically by passing a very thin platinum wire within the aneurysm where the wire coils up to form a yarn-like ball inside the weakened, ballooned-out area of the vessel wall. A clot subsequently forms around the coil and the vessel eventually closes off the opening to what was once the aneurysm.
Fortunately, there is a procedure called “coiling” (Figure 18) which allows most such aneurysms to be successfully treated. Sadly, very people with brain aneurysms know that they have one until it ruptures – by which time it is almost always too late treat it effectively.
Scan Your Troubles Away?
The question logically arises, “Why not look inside everyone’s head if we have the technology to do so? Wouldn’t that allow us to identify not only the people who have aneurysms they don’t know about, but also everyone who has a tumor, or a narrowed coronary or carotid artery, or a gallstone, or anything else wrong with them that they don’t know about? In fact, why not scan their whole bodies and see if anything is amiss? Wouldn’t that allow us to nip most slowly progressing degenerative diseases in the bud?”
The answer to that question is a qualified “Yes and no.” The first and most important qualification to consider is the very substantial difference between them and us. They are going to die and, hopefully, we are not. Once you are content to die, it doesn’t really make a great difference exactly how it happens and it certainly doesn’t make any difference what happens to you afterwards. They will pay exactly nothing to avoid laying around dead for x-hours, or to avoid being autopsied. We, on the other hand, will pay something. That is a huge divide, because, as it turns out, the first and greatest barrier to such universal screening using CT and/or MRI is its adverse cost to benefit ratio.
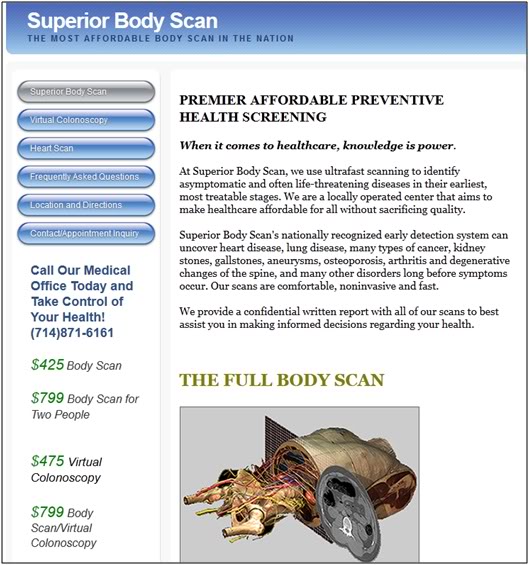
Figure 19: The rapid advance of computing and the high demand for ever more sophisticated medical images has driven the cost of 3-D CT and MRI scanning down to ~ $200 for a head scan $800 for a whole body scan. http://www.superiorbodyscan.com/?gclid=CP_d5Neyiq8CFWwGRQodsHQX-w
While there are many CT and MRI machines, they are kept adequately busy, or perhaps just a little less busy than some of their owners would like, imaging sick and the worried well or hypochondriacal people. If the entire population, or even some modest fraction of it were to suddenly present for imaging, the system would crash. CT and MRI machines are very expensive and while the cost of scans has dropped dramatically, they are still not free. On the macro-level, governments, insurance companies and economists are constantly struggling to determine which therapeutic and diagnostic interventions offer the best return for the money invested in them.
The Problems of Bite Back and VOMIT
Surprisingly, information obtained from diagnostic tests can sometimes not only fail to yield any benefit, in which the case the money spent on the test is wasted, they can also cause harm. A recent example of this, much in the news, is the Prostate Specific Antigen (PSA) test used as a screening tool for prostate cancer (Figure 20). (http://www.pbs.org/newshour/rundown/2011/10/psa-testing-controversy-reignites-over-screening-debate.html) The problem with the PSA test as a screening tool is that to be effective in that capacity it requires a fairly long baseline, a good deal of contextual information (the patient’s race, family history, medications, and so on) and it requires good clinical judgment as well as a ‘patient’ patient.
 Figure 20: It was anticipated that the PSA test, used as a screening tool for prostate cancer, would significantly reduce both the morbidity and mortality from the disease. It has so far failed to do so.
Figure 20: It was anticipated that the PSA test, used as a screening tool for prostate cancer, would significantly reduce both the morbidity and mortality from the disease. It has so far failed to do so.
A single high PSA reading, or even several, may mean nothing. Most often it is the trend, rather than the absolute number; this is particularly true for black men. In short, it’s a test that takes a lot of time and thought to interpret and use well and as such is probably not well suited to mass screening where a “yes” or “no” answer is sought before proceeding to costly, invasive and possibly injurious further evaluation. Yet another problem is that even when prostate cancer is found and treated, it turns out that very few lives are saved because most of those cancers are slow growing and in men who will die of something else before the cancer kills them. Thus, the cost to benefit ratio of the PSA is being questioned, not the least of which because it causes many men to suffer and even die from treatments from which they did not benefit!
This is very much where medicine is today with respect to the “medical imaging singularity.” While it is possible to “look inside” just about everybody, the cost to benefit ratio for the health care system and for the “man on the street” would not justify it. In fact, it would be a medical catastrophe.
To understand why this is so it is necessary to understand three things. The first and most important of these is something called VOMIT, which is a very serious form of bite back associated with our new found ability to see inside patients with increasing exactitude. VOMIT stands for Victim of Medical Imaging Technology and refers to patients who suffer unnecessary interventions for abnormalities observed by imaging or other investigational technology, but which were not found during surgery or subsequent invasive diagnostic interventions. (Hayward, 2003) Here, I will go further and extend the definition of VOMIT to include any diagnostic finding which result in a diagnostic or therapeutic intervention which is not cost effective or causes harm to the patient. That is a very important caveat and tall order to fill, as we shall soon see.
The second is the relatively straightforward one of the ratio of the dollar benefit of resources expended to dollar benefit returned in years of productive life saved as a result of the intervention. Even in cases where early diagnosis saves lives, such as in breast cancer screening, the economic returns are equivocal. It is also often the case that “early” diagnosis with existing imaging technology is still not early enough to cure the disease. As a result, the patient suffers a longer, more miserable course of treatment and the healthcare system is subjected to greater expense with no return.
The third is the problem of information overload and it is somewhat related to VOMIT. The truism that a picture is worth a thousand words is probably a vast understatement. A single 3-D medical image contains a vast wealth of information – information which has heretofore been unavailable to both the clinician and his patient. This might seem like a good thing, and in the long run it will be, but for now, and for a long while to come the details of the landscapes being revealed will, to a great extent, be terra incognito.
The Danger of TMI
When advances in microelectronics allowed for 24-hour ECG monitoring in the 1970s, it became possible for clinicians for the first time to see the beat by beat electrical activity of their patients’ hearts for up to a day at a time, or longer. Prior to that, they were limited by the enormous quantities of paper tracings that would be required and the need to confine the patient to the clinic or laboratory. Now, with the advent of the compact and mobile “Holter monitor,” it was possible to capture the patient’s ECG data continuously under ambulatory, real-world conditions (Figure 21). Physicians were awash in a veritable sea-tide of data!
 Figure 21: The Model 445 Mini-Holter Recorder which was released in 1976 allowed clinicians for the first time to “see” their patients’ ECGs under real-world conditions and for prolonged periods of time.
Figure 21: The Model 445 Mini-Holter Recorder which was released in 1976 allowed clinicians for the first time to “see” their patients’ ECGs under real-world conditions and for prolonged periods of time.
The problem was , they assumed, quite understandably, that they knew what it all meant. After all, doctors had been looking at patients’ ECGs for decades in their offices, in hospitals, at bedsides in homes and in physiology laboratories. They knew how to read an ECG! So, when they discovered that some of their patients had periodic bouts or “runs” of very worrisome arrhythmias, they did the prudent and rational thing – they treated them for these arrhythmias with medications. Unfortunately, the result was the opposite of that expected; a significant increase in morbidity and mortality in these patients, because it turns out that in a subpopulation of healthy people, those arrhythmias were benign and not indicative of any health problem. Thus, misinterpretation of the “same” information they were confident in dealing with in small chunks, presented in bulk and in a different context, was one of the unforeseen and arguably unforeseeable bite back consequences of Holter monitoring technology. (Harrison, 1978)
The Last Heart Attack?
If you assemble and then read over the Alcor case summaries of the last 40 years it is impossible not to be shocked by the seemingly high incidence of sudden and unexpected cardiac arrests. Because my data set is incomplete for Alcor, I can’t be definitive, but the number seems to be somewhat higher than for the same subpopulation of people from the general population (white, middle class, etc). Until, that is, you consider that most cryonicists are male. So, as you read accounts of cryonicists in their 40s and 50s arresting while scuba diving, while taking a nap or watching television, in part what you are seeing is selection bias at work. The point is, no one ever died of “sudden heart disease” a “sudden aneurysm” or, for that matter “a sudden cancer.” These are degenerative disease that takes years to decades to develop. While still difficult to detect in their nascent stages, their terminal lesions are usually very visible many months and sometimes for even for many years before they end lives.
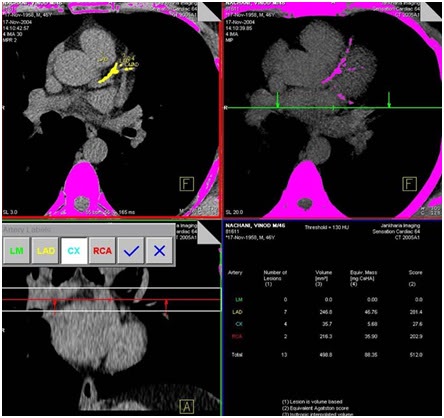 Figure 22: Coronary artery calcium scoring using computed tomography and carotid intima media thickness and plaque using B-mode ultrasonography offer the prospect of detecting almost all coronary artery disease before it reaches the stage where it can cause a heart attack or sudden cardiac arrest.
Figure 22: Coronary artery calcium scoring using computed tomography and carotid intima media thickness and plaque using B-mode ultrasonography offer the prospect of detecting almost all coronary artery disease before it reaches the stage where it can cause a heart attack or sudden cardiac arrest.
There has been a great deal of media attention lately to an initiative called SHAPE; The Society for Heart Attack Prevention and Eradication, which aims to all but eliminate heart attacks by combining CT of the heart to obtain a “myocardial calcium score” (a powerful risk predictor of heart attack)(Figure 22) and carotid intima media thickness and plaque using B-mode ultrasonography as part of a three step program to eliminate heart disease. The next two steps in SHAPE’s plan are a “polypill” combination of blood pressure and anti-atherosclerosis drugs and finally, perhaps, a vaccine. A similar “Last Heart Attack in America” initiative focused on coronary scanning along with dietary interventions to reverse atherosclerosis has been the focus of a feature length documentary on CNN in which former US President Bill Clinton is prominently featured as a spokesman and advocate. The common ground of these two initiatives is that almost no one dies of a heart attack without there being glaring evidence present in their hearts years before the infarct occurs. It is only necessary to look for it!
There can be no question that as imaging technology evolves, and as medical acumen catches up with what is available, that such imaging will become a routine part of any checkup for patients whose age and risk profile merit it (and eventually, if they live long enough, that means most patients). As it stands right now, if you are a middle aged man or woman with a significant risk profile for heart disease, and you have a heart attack, it’s my personal opinion you have ample grounds to sue your physician for negligence. Right now, that’s just my opinion, so it doesn’t count for anything, but the point is that sooner or later this, or a better coronary imaging modality is going to become the standard of care and heart attacks will become a rare event – a thing of the past – a relic from a time when doctors couldn’t see inside of you.
Ultrasound Investigations
There are cheaper, simpler and completely risk free ways (in terms of radiation) to find out whether you have atherosclerosis or not. The most predictive of these for money is the carotid ultrasound (CUS) test.
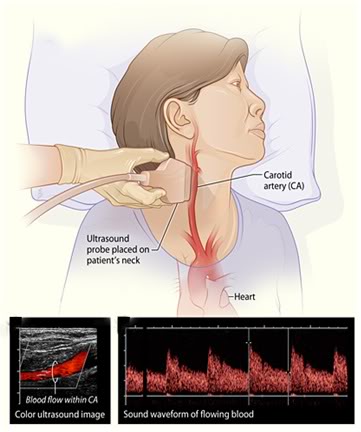
Figure 23: The carotid ultrasound scan is a simple, non-invasive diagnostic investigation that employs sound waves to create an image of the two large blood vessels in the neck that supply most of the blood to the brain. If there is a buildup of plaque or a thickening of the limning of these two arteries the person is at increased risk of stroke and there is a high probability that there is also systemic atherosclerosis present. If there is evidence of severe narrowing of one or both of the vessels, then it becomes urgent that medication and possibly surgery be used to correct the condition in order to avoid the likelihood of a crippling or lethal stroke.
This simple, non-invasive test takes just a few minutes and uses ultrasound waves to image the carotid arteries and the blood flowing through them (Figure 23). If there is thickening of the arterial wall, or plaque present, then it is a virtual certainty that the person has systemic atherosclerosis and warrants a more extensive workup. This test is often also “packaged” with a quick “look-see” at the abdominal aorta also using ultrasound, to rule out the possibility of an abdominal aortic aneurysm – something that is more common in smokers once they reach middle age, and beyond.
If you shop around diligently, the cost a CUS can be as little as your transportation costs to the health fare or community center where it is being offered, often as a “loss leader” by health care providers or medical imaging companies seeking more remunerative business opportunities (if they find something amiss during the CUS). The cost of such an evaluation can range from as little as $60, to as much as $380.
A CUS is ideal for people on a budget and for those under age 45 with no history of heart disease, cancer or other pathology or risk factors that might put them at increased risk of sudden cardiac arrest.
Why Full Body Scans?
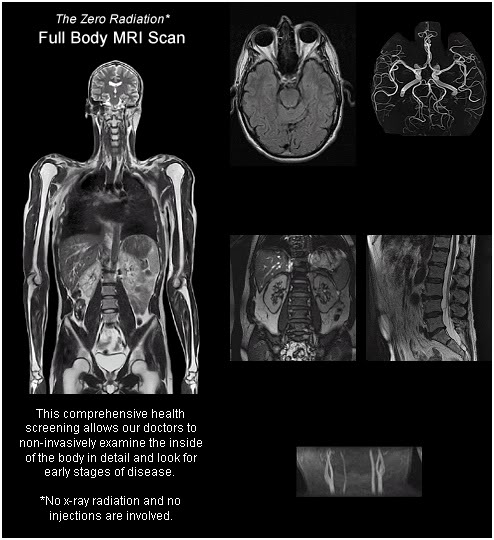
Figure 24: The full body CT or MRI scan is often offered as “add-on” to the complete or the “executive’s” physical. Many imaging centers offer these scans without the need of the patient’s person physician prescribing the scan using their in-house radiologists to write the order for the test. http://www.prevenium.com/contact.asp
Put simply, there is no substitute for seeing, or to put a new twist on an old adage: a picture is worth a thousand medical tests. While the origins of all of the degenerative diseases that kill us are at the molecular level, mostly we die as a consequence of the macro-level changes they inflict on our bodies, even if the coup de gras is rooted in the action of things like adhesion molecules and inflammatory pathways; as is the case with most heart attacks. It is the large, easily “seen” bulges of aneurysms, masses of plaque or tumor that kill, and these almost always take years to develop. What this means practically is that, with a few exceptions, aside from suicide, homicide and accident, virtually no one has to die – or to deanimate without plenty of advance warming. The implications for cryonics are as obvious as they are profound.
End of Part 3

Time to schedule my full body MRI.
No, you shouldn’t do that, certainly not until the series of articles is complete. There is real risk of injury and death from pursuing scans in other than the proper way. THIS IS NOT THEORETICAL, it is a demonstrated fact in a wide range of other screening procedures, ranging from the humble PSA test, to more sophisticated imaging tests.
Imaging data can be lethal – I’ve seen a number of cases myself and seen many more discussed in professional medical forums. We do not yet know how to interpret the data we are seeing coming from healthy (or asymptomatic) people. There is a solution to this problem, but it requires foreknowledge and discipline. It will be discussed shortly.
Literally just a few days ago, and elderly cryonicist who was scanned to get his cardiac calcium score was found to have inflammation and some mucus plugging in some areas of one lung as an incidental finding. He is clinically well. A BAL procedure was suggested. I can tell you straight-up that if you do BALs on 100 patients in his age and medical condition, you will likely seriously injure or kill one or two of them. Nothing in his scan suggests any possible useful intervention that would not be just as possible or useful should he become symptomatic. He did not have the BAL and it has been several weeks and he remains well.
Ideally, (as I point out in a future segment) DSSing would be done in an institutional framework (one I was hoping to create, alas now postponed). In fact, arguably, it is the only way to do it. If I had know circumstances (for me) were to have changed so suddenly in the last 24 hours, I would have withheld this information and not run this series of articles at all. But, I’ve started, and it is unarguably more hazardous to stop than to proceed.
I’ve given consideration to running all of the remaining components at once. However, it has been my experience that this results in a) complaints about too much to read at once, b) people not reading and absorbing the material incrementally, as it was written to be read.
I’ll also give consideration to pulling the existing articles and possibly bundling the entire article into a PDF which will be available on-line. I’m not sure about this yet.
Finally, this idea is one which I’ve been considering and working on for several years. I spoke with a number of experts in medical imaging, in the ethics of screening interventions and attempted elicit help from a range of professionals in and out of the cryonics community (unsuccessfully). I did this because I’ve seen medical imaging maim and kill healthy people. I was also a first-hand witness to the “Holter monitor” fiasco of the 1970s, where hordes of patients were placed on antiarrhythmic drugs only to be injured or killed by them. I took over a year to (I hope) carefully weigh the risks vs. the benefits of DSSing.
Ultimately, there is no way to know until you do the experiment. Having said that, it is incumbent upon all involved to pursue this “experiment” in a responsible fashion, avoiding known pitfalls. And it IS an experiment. And there will be bite back. There always is. — Mike Darwin