Section 3:
Perfluorchemicals (PFCs)

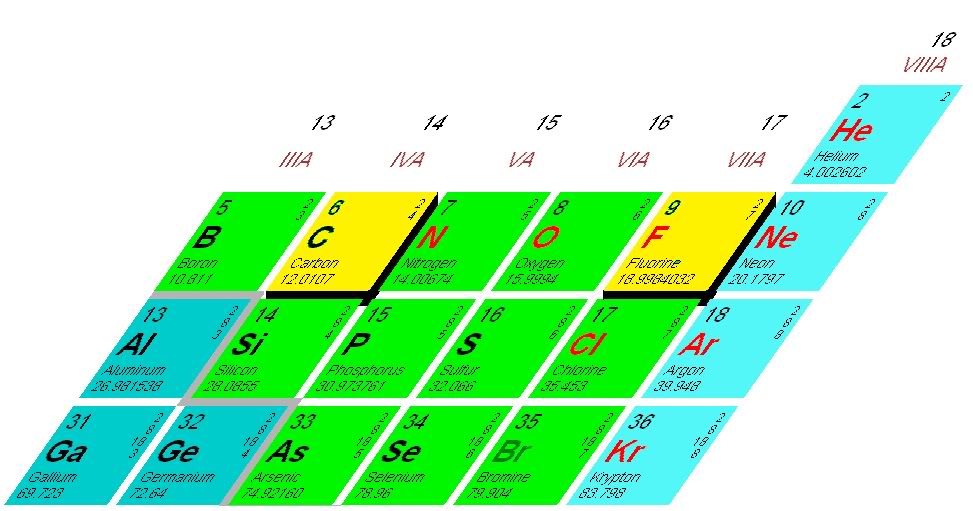
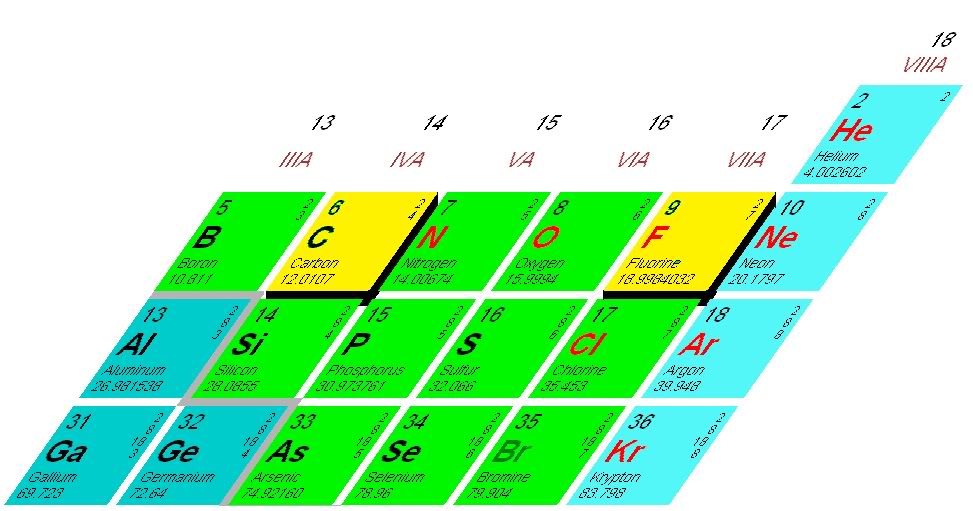
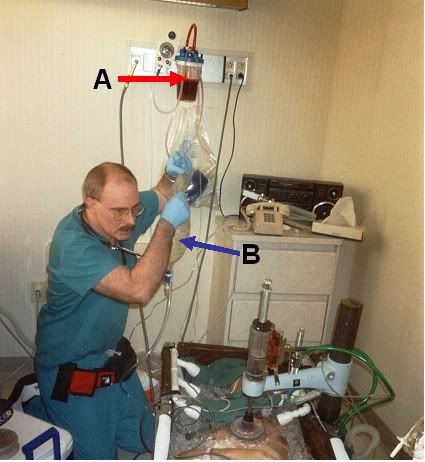
Figure 3-1: Fluorine and carbon; the two building blocks of the remarkable molecules knows as the perflurochemicals (PFC)s.
Physical Chemistry and Synthesis
Perfluorchemicals (PFCs) are derived from hydrocarbons by replacing hydrogen atoms with fluorine atoms, typically using common organic hydrocarbons as substrates. This is accomplished by one of three methods; the oldest of which is via a highly exothermic vapor-phase reaction employing fluorine gas. An alternative method is the more stable cobalt trifluoride technique which was developed during the Manhattan Project in World war II (WWII) [290]. Electrochemical fluorination, developed by Simmons in1950 [291] has increasingly replaced the earlier techniques.
Ectrochemical fluorination yields more homogeneous products with less carbon-carbon bond cleavage and is better suited to smaller scale production of molecules for use in research and development applications. However, whether done by electrolysis or by using the pre-Simmons method of reaction with high-valent metal fluorides, both laboratory and industrial scale PFC manufacturing and synthesis have in the past resulted in impure and poorly characterized compounds (unless perfluorinated building blocks are employed as starters). This occurs because the large difference (~15 kcal per M-1) in the carbon-hydrogen bond versus the carbon-fluorine bond energies (and the release of this energy during the synthetic process) results in undesired side reactions, isomerisations, and polymerizations creating a mélange of compounds which are not fully characterized, let alone purified.[292]
PFC carbon chain length is variable, and these, in addition to the attached moieties, determine the individual properties of a given molecule. Liquid PFCs that are useful as gas and/or heat exchange media in the lungs all exploit the utterly unique properties of the carbon-fluorine (C-F) bond and the larger size of fluorine atoms compared to hydrogen atoms. The C-F bond is the strongest covalent bond found in organic chemicals (average 485 kJ mol-1, compared to ~413 kJ mol-1 for a standard C-H bond) [293] and this bond-strength is amplified as the number of fluorine atoms on each carbon atom increases.[293]
The electroattracting nature of the fluorine atoms further increases the strength of the C-C bonds and the larger size of fluorine atoms (estimated van der Waals radius of 147 versus 120 pm) [294] and their high electron density result in a compact electron shield that ensures effective protection of the molecule’s backbone. The dense electron shell of the fluorine atoms may also provide protection against nucleophilic attack. The PFCs thus have very high intra-molecular (covalent) bonding and very low intermolecular forces (van der Waals interactions).[295]
Physical Properties
These liquids are clear, colorless, odorless, non-conducting, nonflammable, and are both hydrophobic and lipophobic. Replacement of hydrogen atoms by fluorine atoms results in high thermal stability and chemical inertness. PFCs do not undergo decomposition (except at temperatures above ~350ºC) and they are not metabolized or acted upon by any enzymatic system. They are ~1.8 times as dense as water; and are capable of dissolving large amounts of physiologically necessary gases (45 to 55 ml O2/dl and16 to 210 ml CO2/dl).[296] O2 dissolution in PFCs is via O2 occupying intermolecular sites in the liquid, unlike the pH and concentration dependent porphyrin binding in hemoglobin which is responsible for the sigmoidal oxyhemoglobin dissociation curve.[297] O2 solubility in PFCs is a linear function of the pO2 (per Henry’s law) and the structure of the particular PFC.[298] Solubility of O2 and other gases in PFCs is a function of the NMR T1 relaxation constant which determines the intermolecular cavity size and the presence and character of large channels within the liquid. Linear aliphatic structures more easily allow the formation of such channels while planar structures result in more closely interlocked layers which accommodate less gas. While the solubility of O2 is greater in aliphatic than in aromatic PFCs this is not the case with CO2. O2 solubility increases with the degree of fluorination and the O2-dissolving capacity of aliphatic PFCs having 9-11 carbons is in the range of 40 to 60 mole fractions of O2, or roughly twice that of aromatic molecules.
The O2 content of perfluocarbons at 1 atmosphere (atm) of 100% O2 is approximately 20 times that of water, twice that of blood, and 1.5 times that of an equal volume of gaseous O2. If the PFCs are compared to blood in terms of O2 carrying capacity under normal atmospheric conditions it is immediately obvious that PFCs carry only a fraction of the O2 that hemoglobin does. However, it is not simply the O2 dissolving capacity of PFCs that is important, but also their O2 delivery capability. The O2 diffusion rate from the PFC-filled alveoli to the alveolar capillaries is quite high when saturated with O2 at 760 torr [299] and due to their 50% greater O2 carrying capacity than O2 delivered as a gas at an FiO2 of 100%, the delivered O2 to the blood is 25% to 50% greater than is possible using 100% gaseous O2 for ventilation. The use of such a high FiO2 is sustainable with PFCs because, for reasons not yet understood, O2 toxicity does not occur in their presence as a liquid in the lung under normobaric conditions.
A remarkable and essential feature of the PFCs in liquid assisted ventilation is that they are essentially insoluble in both water (7 to 11 ppm at STP) and alcohols, and are only sparingly soluble in some lipids.[299] The PFCs have a kinematic viscosity (ratio of viscosity to density) similar to that of water [300] and an extremely low surface tension (15 to 19 dyn/cm2) and dielectric constant; again secondary to weak intermolecular forces resulting from the exterior fluorine atoms.[301] The volatility of PFCs varies widely depending upon the molecular weight of the molecule, with vapor pressures ranging from ~1 to over 80 torr at 25ºC. Vapor pressure is the critical determinant of the half-life of elimination of a given PFC from the lungs following both intrapulmonary and intravenous administration. Vapor pressure also dictates the viscosity of a given PFC and thus PFC-gas and PFC-surface shear interactions.[302],[303] Vapor pressure is also a critical determinant of toxicity as will be discussed under the heading Toxicology, below.
Commercially Available PFCs
Historically, the requirements of a PFC for use as a gas exchange medium in liquid ventilation are excellent solubility for respiratory and putative therapeutic gases such CO, NO, and H2S, kinematic viscosity in the range of ~ 0.50 to 2.2, low to moderate vapor pressure (1 to 15 torr) with a cutoff of 20 torr, a high spreading coefficient and a very low surface tension.[303] Additionally, a PFC that is to be used for intrapulmonary heat exchange must have a viscosity and freezing point appropriate to the application. These criteria, particularly with respect to vapor pressure and viscosity, may change in the future, depending upon the application, medical condition being treated, or large airway diameter of the patient.
No existing PFC combines all of these desirable properties, and certainly no single PFC can be tailored to have the widely varying physical properties required for a particular pathology or patient. In addition, from a physical chemistry standpoint, no single PFC is likely to combine all these properties, even in the sphere of providing assisted ventilation in ARDS; and recent research has begun to focus not only on the creation of novel of PFCs for liquid assisted ventilation applications, but also on investigating mixtures of different PFCs to provide an optimum ventilating medium which can be formulated to meet the needs of a given application.[304]
Unfortunately, de novo flurochemical synthesis involves the use of extremely toxic and hazardous materials such as fluorine gas, hydrogen fluoride, silver difluoride, or the halogen fluorides, and yields a poor ratio of desired end product to undesired (and costly to dispose of) side-products and waste.[293] Even flurochemical synthesis using per- and poly-fluroinated reagents, the ‘building block’ approach is costly, has low selectivity for many compounds and requires formidable expertise [305], although this is changing.[306]
Once the synthesis is completed, numerous and costly purification steps such as lengthily refluxing, spinning band distillation and reparative vapor phase chromatography must be undertaken, adding greatly to the cost, and making well characterized synthesis and purification of quantities sufficient for use in liquid assisted ventilation or blood substitutes a full-time effort and the province of expert chemists and dedicated facilities.[293] Historically, this has severely limited the development and commercial production of high purity, completely chemically characterized novel PFCs.
As a result, most of the initial work in liquid ventilation (including that done for liquid assisted pulmonary cooling (LAPC)) was carried out using commercially available PFCs such as perflurodecalin, Rimar-101™ (Miteni Corporation, Milan, Italy), or the Fluorinert™ liquids (3M Company, St. Paul, MN). Table 3, below, shows some of the physical properties of a number of commercially available PFCs used for leak testing, heat exchange and for cleaning applications in the electronics industry marked by 3M Corporation as the Fluorinert™ ‘liquids,’ as well as those of Rimar-101 and Perflubron™ (Alliance Pharmaceuticals, San Diego, CA).
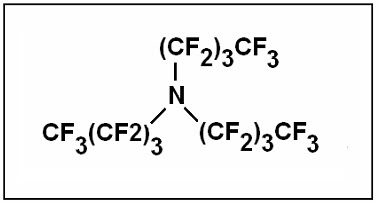
A serious disadvantage to Fluorinert™ PFCs and all other industrial grade PFCs (as well as most reagent grade materials available from laboratory chemical suppliers) is that they are not chemically defined in terms of chain length or even precise chemical composition. As examples, FC-75 has been shown to have as many as 6 peaks when evaluated by gas chromatography and F-tripropylamine (FTPA), one of the components in the first FDA approved blood substitute, Flusol-DA, contained only 27% of perfluorinated FTPA in addition to a number of other uncharacterized compounds.[307] FC-43, a PFC used extensively as an experimental oxygen carrying blood substitute and for liquid assisted ventilation is chemically ~ 85% perfluoro-tri-n-butylamine (C12F27) with the unit structure shown in Figure 3-2. However, the perfluoro-tri-n-butylamine molecules may be present as polymers of varying lengths, and other related fluorinated molecular species are also present.
The degree of polymerization as well as the physical properties of the species which comprise the ~15% balance of FC-84, are such that the average vapor pressure, boiling point, melting point, thermal conductivity and other physical properties of FC-84 are fairly uniform from lot-to-lot.[308],[184] However, two of the most critically important determinants of the utility of PFCs in liquid ventilation applications are their vapor pressure (and thus their viscosity) and their direct chemical toxicity. Vapor pressure is of great concern, because even if the average vapor pressure of the liquid is quite low (i.e., 1.3 torr at STP for FC-43) if even a small percentage of the species present have a far higher vapor pressure, then that fraction of the liquid can turn into a gas and create long-lasting and mechanically disruptive bubbles in lung tissue under conditions of baro- and/or volu-trauma; and will create ‘sponge rubber lung’ syndrome due to stable intra-alveolar gas bubble formation by vaporizing between surfactant and the alveolar epithelium. This phenomenon, known as hyper-inflated non-collapsible lungs (HNCL) occurs even under the relatively non-traumatic conditions of PLV if the vapor pressure is low enough; as is the case with F-alkylfuran in FC-75.[309] Similarly, the unspecified and often uncharacterized other perflurocompounds (or even incompletely fluorinated compounds) may be chemically toxic to cells.[310],[311],[292]
Some Perfluorchemicals Used in Liquid Ventilation Research
|
| Physical Property |
FC-40
|
FC-43
|
FC-75
|
FC-
77
|
FC-84
|
PFOB
|
PP5/6
|
Rimar-101
|
PP50
|
|
Boiling Point (°C)
|
155
|
174
|
102
|
97
|
80
|
140.5
|
142
|
102
|
142
|
|
Pour Point (°C)
|
-57
|
-50
|
-80
|
-95
|
-95
|
-6
|
-8
|
|
-8
|
|
Vapor Pressure (torr)
|
3
|
1.3
|
31.5
|
42
|
79
|
5.2
|
6
|
31.6
|
6
|
|
Density (kg/m3)
|
1.87
|
1.88
|
1.77
|
1.78
|
1.73
|
1.93
|
1.917
|
1.78
|
1917
|
|
Coefficient of Volume Expansion (°C-1)
|
0.0012
|
0.0012
|
0.0014
|
0.0014
|
0.0015
|
|
0.00104
|
|
2.66
|
|
Kinematic Viscosity (cSt)
|
2.2
|
2.8
|
7.4
|
0.8
|
0.55
|
1
|
2.66
|
0.82
|
2.61
|
|
Absolute Viscosity (centipoise)
|
3.4
|
4.7
|
1.4
|
1.3
|
0.91
|
1
|
|
1
|
|
|
Specific Heat (J kg-1 °C-1)
|
0.25
|
0.25
|
1050
|
0.25
|
0.25
|
|
1.05
|
|
1.05
|
|
Heat of Vaporization @ B.P. (J/g)
|
17
|
17
|
88
|
20
|
19
|
|
78.7
|
|
78.8
|
|
Thermal Conductivity, watts (cm2) (°C/cm)
|
0.0006
|
0.0006
|
0.0006
|
0.00063
|
0.0006
|
|
57
|
|
0.00057
|
|
Surface Tension (dynes/cm)
|
16
|
16
|
15
|
15
|
13
|
18
|
17.6
|
15
|
19.3
|
|
Solubility of Water (ppm)
|
7
|
7
|
7
|
13
|
11
|
<10
|
<10
|
<10
|
|
|
Solubility of Air (ml gas/100 ml liquid)
|
27
|
26
|
25
|
41
|
43
|
|
|
|
|
|
Solubility of O2 (ml/100 ml liquid) @ 25ºC
|
50
|
52
|
52
|
50
|
|
52.7
|
49
|
52.2
|
49
|
| Solubility of CO2 (ml/100 ml liquid) @ 37ºC |
|
|
160
|
108
|
|
210
|
140
|
160
|
140
|
| Molecular Weight |
650
|
670
|
416.06
|
415
|
388
|
499
|
462
|
416.1
|
462
|
|
Table 3: Physical properties of some PFCs that have been used for liquid assisted ventilation: 3-M Fluorinert Liquids ™, Rimar-101, perflurodecalin and perflurooctylbromide (PFOB, Perflubron™). Perflubron™ is the first completely defined PFC intended for medical applications. Sources: [312],[292] ,[313].
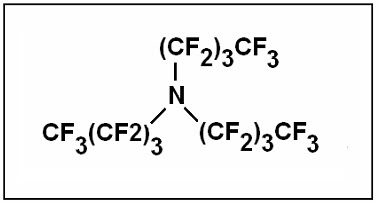
Figure 3-2: Chemical structure of perfluoro-tri-n-butylamine (FC-43).
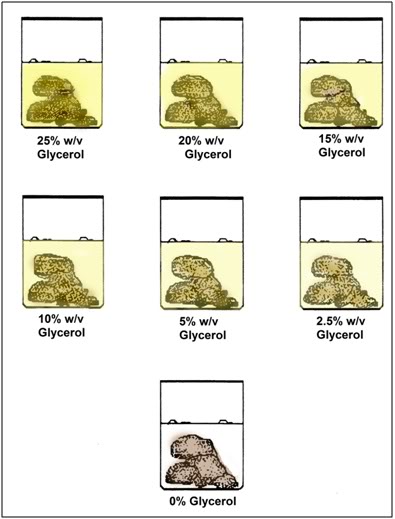
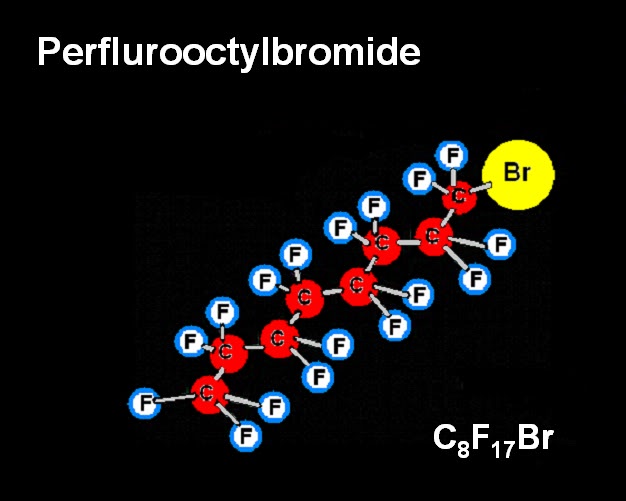
For these reasons a completely chemically defined molecule, perflurooctylbromide F3(CF2)7Br, Perflubron,™ LiquiVent™), was developed by Alliance Pharmaceuticals of San Diego, CA for use in clinical trials of liquid ventilation (Figure 25, below). Unfortunately, Perflubron™, (Figure 3-3) with a molecular weight (MW) of 498.97, has a freezing point of +6.0ºC which makes it unsuitable for use in inducing ultraprofound hypothermia (0-5oC) where the temperature of the ventilating liquid must be in the range of 2ºC to 4ºC for optimum efficacy.
Toxicology
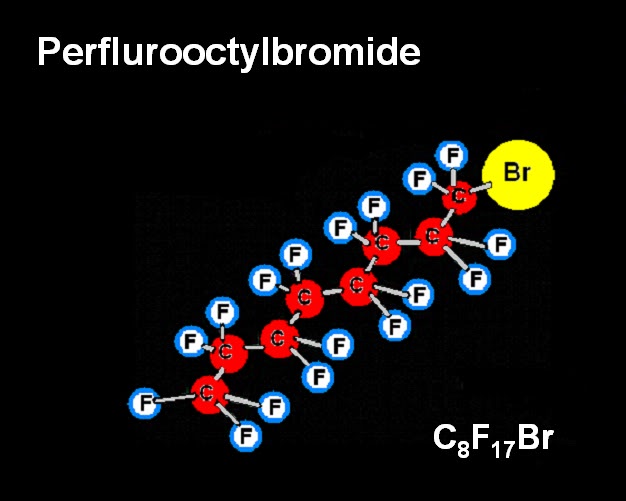
Figure 3-3: Perflurooctylbromide (LiquiVent™)
The high stability, chemical inertness, and nearly total insolubility in both water and lipids of PFCs used in liquid assisted ventilation preclude their metabolism and limit their interaction with biomolecules. Despite 40-plus years of use in biomedicine little published work has been done on the toxicology of these compounds. Based on data from the available literature their toxicity can be divided into two categories: biophysical/biomechanical and immunological. When administered intravenously or intraperitoneally as neat (pure) chemicals injury results from the biophysical interaction with the animal rather than from biochemical interactions. Because PFCs are not miscible in water they form vascular emboli in the same way that injecting intravascular oil or air would.
PFCs with higher vapor pressures can form vascular gas emboli even if emulsified [314] and can lethally distend closed body viscuses such as the peritoneum, or cause perfluorocarbon vapor pneumothoraces (‘perflurothorax’).
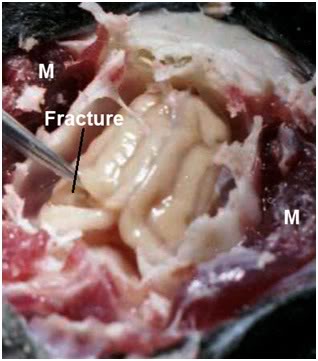
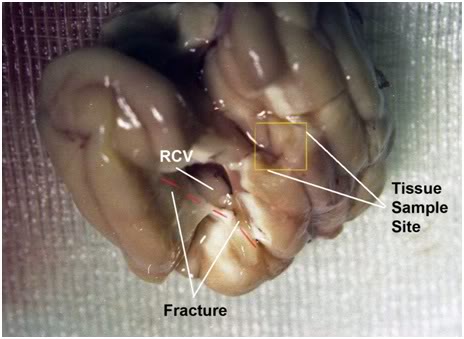
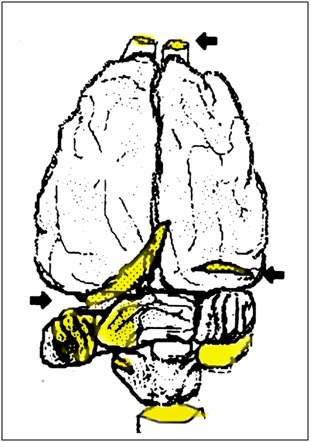
PFCs of intermediate vapor pressure may accumulate in the lungs and be converted to vapor which is retained for weeks or months in the alveoli or lung parenchyma resulting in what Clark, et al., termed hyperinflated non-collapsible lungs (HNCL). [309] This phenomenon is noted at necropsy after IV administration of emulsified perflurodecalin containing blood substitutes [315] and after LAPC with intermediate vapor pressure PFCs such as FC-75 or FC-77.[272] Schutt, et al., call this ‘pulmonary alveolar gas trapping’ and they propose that the phenomenon occurs as a result of PFC liquid or vapor migration through the pulmonary surfactant-liquid bridges where it forms stable, long lasting, PFC vapor micro-bubbles. They propose that these intra-alveolar micro-bubbles are part of the ‘normal pulmonary elimination of perfluorocarbon vapor’ from the body.[316] While HNCL or ‘pulmonary alveolar gas trapping’ may not be clinically evident, and does not perturb blood gases or interfere with gas exchange, it does interfere with normal respiratory mechanics and can cause ‘stiff lungs’ in dogs following LAPC using FC-75 or FC-77.[161],[272] Stiff lungs increase the work of breathing until the vapor dissipates enough to relieve the acute tension in the alveoli.[272] As such, the author believes this phenomenon should properly be classified as an adverse biophysical effect, rather than an acceptable or normal mechanism of PFC elimination. It is interesting to note that in a chemical model of lung injury using inhaled kerosene even brief PLV with FC-77 increased mortality and resulted in extensive gas trapping.[317]
Depending upon the emulsion size intravascular PFCs may be phagocytized by PMNL’s and macrophages and be deposited in the reticuloendothelial system where they may cause enzyme induction or mild inflammation from their space occupying, mechanical effects distorting normal tissue architecture. [318] These changes are typically reversible as the PFC is eliminated via the lungs and the hepatomegaly and splenomegaly dissipate (~ 3-weeks).
The immunological effects of PFCs vary with the molecule, method of preparation and particle size (if administered intravascularly). Some PFCs appear to be directly cytotoxic to PMNLs and macrophages.[319] However, as a class, the PFCs seem to interfere with PMNL and macrophage chemotaxis, activation and de-granulation without inducing apoptosis or necrosis, by mechanisms that are not understood.[320], [321],[322] Augustin, et al., have observed that PFCs alter the cytoskeleton of hepatic macrophages in a dose dependent manner that varies with the compound. [323] Inhibition of PMNL and macrophage chemotaxis and respiratory bursts gives the PFCs moderately potent anti-inflammatory effects and by the same token makes them immunosuppressive. While this effect is immunomodulatory and probably beneficial in ARDS [324],[325],[326], it also has the potential to impair pulmonary and systemic immune surveillance and presumably increase the risk of infection and neoplasm. FC-43 has been used to delay neutrophil mediated xenograft rejection [327],[328] and Perflubron™ has been demonstrated to inhibit neutrophil activation in the rat heart after 2-hours of cold ischemia and whole blood reperfusion.[329]
A recently discovered novel and unexpected effect of at least one PFC, Perflubron™ [326], is direct inhibition of oxidative damage in both cultured pulmonary artery endothelial cells exposed to hydrogen peroxide and in linoleic acid micelles subjected to varying concentrations of the azo initiator 2,2’-diazo-bis-(2-amidinopropane) dihydrochloride . This result is unexpected because it has previously been presumed that the antioxidant activity of PFCs was secondary to their immunomodulating and immunosuppressive effects. The protective effect of Perflubron™ in a non-biological system raises many questions about its basic pharmacology, and possibly about the chemistry and environmental interactions of the PFCs as a class, should this effect prove replicable with similar compounds.
Environmental Impact and Future Availability
The PFCs may be justifiably described as the penultimate atmospheric (greenhouse) poison. The PFCs, like water vapor and methane, both absorb and emit long wave (infrared) radiation; effectively trapping heat from the sun and warming the terrestrial surface and atmosphere.

Unlike CO2 and methane, PFCs are not subject to biological cycling, are unaffected by electrochemical reactions, and do not dissociate in aqueous media. They are essentially already fully oxidized and are unaffected by standard oxidizing agents such as permanganates, chromates, and the like. As previously noted, degradation via oxidation occurs only at very high temperatures. Because of their inertness, they are similarly resistant to degradation by reduction, except under extreme conditions, requiring reducing agents such as metallic sodium. This leaves photochemical decomposition, primarily via hydroxyl radical (.OH) mediated degradation, as the only means of terrestrial disposition. Both Cicerone [330] and Yi Tang [331] have shown that the reaction of .OH with the C3 and CF4 moieties is negligible under ground-state conditions, and that the lifespan of the molecules, once they enter the atmosphere, is likely in excess of 10,000 years. The heavier, higher MW and lower vapor pressure PFCs which are ideal for liquid assisted ventilation can be expected to remain in the lower reaches of the troposphere indefinitely, and thus not reach the upper atmosphere where, however slowly, they might be photo-degraded. In any event, the PFCs are so resistant to photo-degradation that the Flourinerts, and related compounds that are used as chemically stable cooling agents in photochemical reactors, as carrier solvents for photo-decomposition of other organic molecules, and are likewise classed as ‘radiation durable compounds’ for use in the photolithography industry.[332]
At present, the PFCs constitute an insignificant contribution to greenhouse gas emissions. However, widespread medical use could change this, and in any event, 3M, DuPont and other manufactures of industrial quantities of PFCs are aggressively encouraging the use of alternative compounds which they manufacture, principally the hydrofluoroethers [333] and the perfluorinated alkyl vinyl ethers. In 1982 Riess and Le Blanc estimated that if PFC-based blood substitutes came into wide use the quantities required would be in the ‘multi-thousand-tons-per-year range’ [292] all of which would end up in the atmosphere. Widespread use of PFC-facilitated LAPC and PLV could easily require a similar amount of product.
Extensive medical use of PFCs would seem to mandate associated efforts at recovery and recycling to minimize environmental contamination. However, this is not easy to do even in hospital under controlled conditions. Recovery of PFCs used emergently for LAPC (i.e., in-field induction of hypothermia in stroke, myocardial infarction, cardiac arrest) and as the O2 carrying molecules in blood substitutes would seem to preclude effective recovery. The indefinite lifespan of these compounds makes their use akin to radiation exposure wherein the effect is cumulatively damaging, and ultimately lethal to the biosphere (as it exists now) as a consequence of their greenhouse effects and indefinite atmospheric lifespan.
The PFCs used in liquid assisted ventilation do not seem likely to accumulate or concentrate in biota. However, they do have comparatively long dwell times in patients when used clinically, and the exposure of health care workers to these volatile compounds would seem unavoidable. In light of these facts and the recent discovery that PFCs have direct radical quenching effects (with possible important environmental ramifications), as well as immunosuppressive properties, it seems reasonable to question the future large scale production, and thus the biomedical availability of these molecules.
Section 4:
History of Liquid
Assisted Ventilation and Implications for LAPC

History of Liquid Ventilation

Figure 4-1: An ultra-deep sea diver breathing PFC liquid in the 1989 motion picture ‘The Abyss’ Directed by James Cameron. [Photo courtesy 20th Century Fox and Lightstorm Entertainment.]
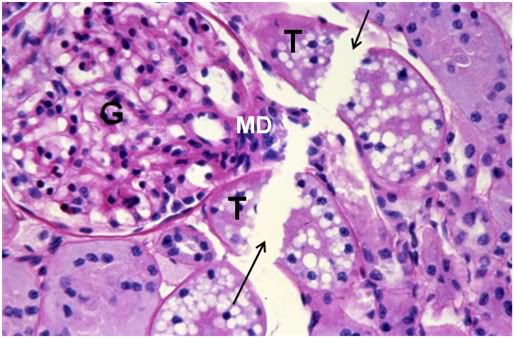
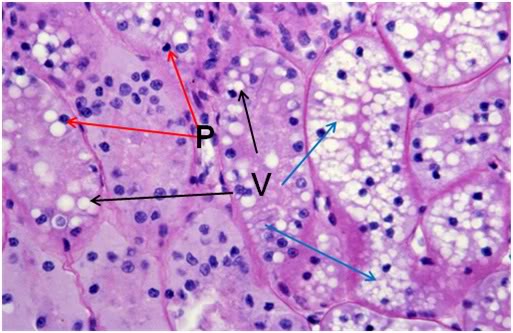
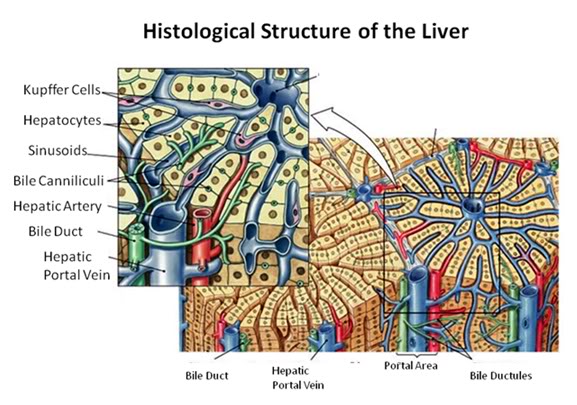
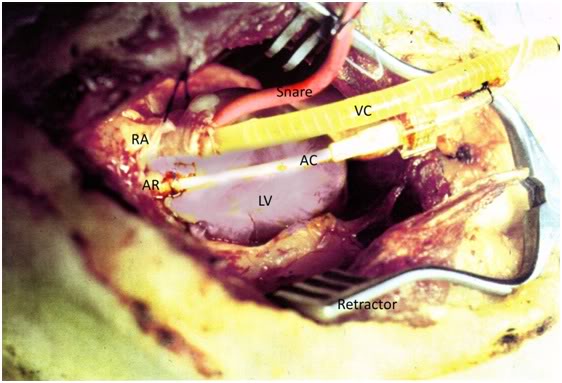
As was the case with the first great rationalization of surgery and wound management by Pare’ [352], the creation of scientific nursing by Nightingale [353], and the development of fluid resuscitation and the first effective medical management of shock by Cannon [354] and Blalock [355], the impetus for the development of liquid ventilation was also initially warfare. Interest in the use of liquid as a breathing medium in mammals originated in the early 1960s in response to the U.S. Navy’s need to develop rescue systems for submariners that would allow them to transiently breathe saline or some other aqueous liquid. Mortality among submariners in World War I (WWI) and WW II was greater than in any other branch of military service. In WWII 22% of U.S. and 75% German submariners were killed in action.[356] With the advent of nuclear submarines in 1951, and the use of submarines to carry and deliver nuclear weapons, prolonged and complex missions while continuously submerged created the need (still largely unmet) to carry out rescue of submariners, and recovery of nuclear weapons and other strategically critical materiel, from extreme depths.
Johannes Arnold Klystra, M.D. is the Dutch pulmonologist and clinical researcher responsible for developing saline lavage of the lung as a treatment for advanced cystic fibrosis in 1958.[357] Klysta’s interests extended well beyond clinical innovation in the management of lung diseases, and in the late 1950s this maverick physician approached the Dutch Navy to explore possible ways to allow deep ocean recovery of submariners as well as the development of liquid breathing systems that would allow divers to be free from the constraints imposed by gas breathing under conditions of high pressures (Figure 4-1):
“Man has tried for centuries to invade the oceans, perhaps driven by a subconscious nostalgia for atavistic weightlessness in the vast hydrosphere that covers more than 70 per cent of the earth, but gas in his lungs, compressed by a layer of water above, confines his activities to the shallow. Nitrogen, for instance, produces a progressively severe intoxication at depths greater than100 feet and usually incapacitates a diver by ‘rapture of the deep’ at no more than300 feet. Moreover, relatively large amounts of carrier gas dissolve in blood and tissues to be released as bubbles whenever the diver returns to the surface too rapidly. These hazards are all due to the compressibility of gases. The properties of water, on the other hand, hardly change at all with pressure, and I have observed mice with fluid filled airspaces move around in no apparent distress at a simulated depth of 3000 feet. If man were able to breathe oxygenated water instead of an oxygenated carrier gas, exploration of the oceans would no longer be limited by gas toxicity and decompression sickness.”[358]
The first mammal to survive liquid breathing was a mongrel dog named ‘Snibby.’ [158] Snibby was shaved, bathed, anesthetized, intubated, and submerged in a tub of buffered salt solution in a large hyperbaric chamber at 5 atmospheres of pressure while O2 was bubbled through the saline bath. The dog breathed the liquid, which was held at a temperature of 32ºC, for 24 minutes. As Klystra noted in his published account of the experiment: “Snibby’s recovery was uneventful and he was adopted by the officers and crew of H. M. Cerberus to serve as a mascot aboard this submarine rescue vessel of the Royal Netherlands Navy.”[359]
In 1962 Klystra documented survival of mice breathing a balanced, buffered salt solution under 8 atmospheres of pressure at 20ºC for 18-hours.[158] Throughout the 1960s Klystra and his associates probed the limits of liquid breathing using aqueous solutions and they were the first to document the problem of profound hypercarbia as a fundamental limitation in tidal liquid breathing.[157] Klystra was also the first to demonstrate survival of mammals following extreme hyperbaria using spontaneous liquid breathing of a buffered salt solution.[357] A further testimony to the highly creative and innovative nature of Klystra’s work was his use of the selectively liquid lavaged lung lobe as a possible replacement for the kidney; in other words, as a mass exchanger for nitrogenous wastes and as an osmotically driven ultrafilter for removal of excess water in the setting of renal failure.[360]
One of the most remarkable things about this pioneering work is that saline and other aqueous solutions denude the alveoli of surfactant, the stiff molecular cage that supports the 3-dimensional alveolar structure and keeps the acinar airways open to ventilation. Removal of surfactant is a primary cause of serious pulmonary injury and a major pathophysiological mechanism in both acute lung injury (ALI) and the acute respiratory distress syndrome (ARDS). Through the present, saline lavage of the lungs remains a standard model for inducing pulmonary injury to simulate ALI and ARDS in experimental animals.[361],[362] The inadequate gas carrying capacity of aqueous solutions under normobaric conditions, and the inherently injurious nature of water-based ventilating media made clinical or undersea application of liquid breathing infeasible. Indeed, breathing of balanced salt solutions, even under hyperbaric conditions in the presence of 100% O2 was only possible for extended periods of time if the animals were hypothermic. While O2 delivery was adequate, CO2 elimination was not, and hypercarbia and respiratory acidosis were lethal complications of liquid breathing under normothermic conditions.[363]
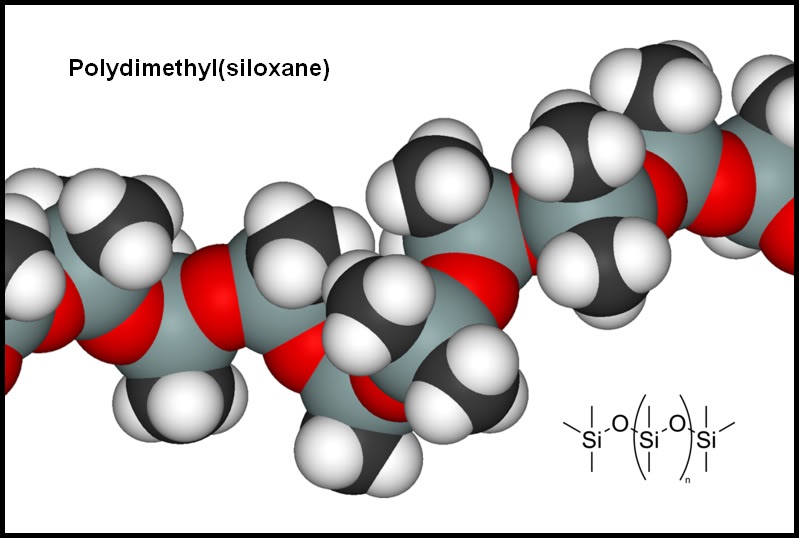
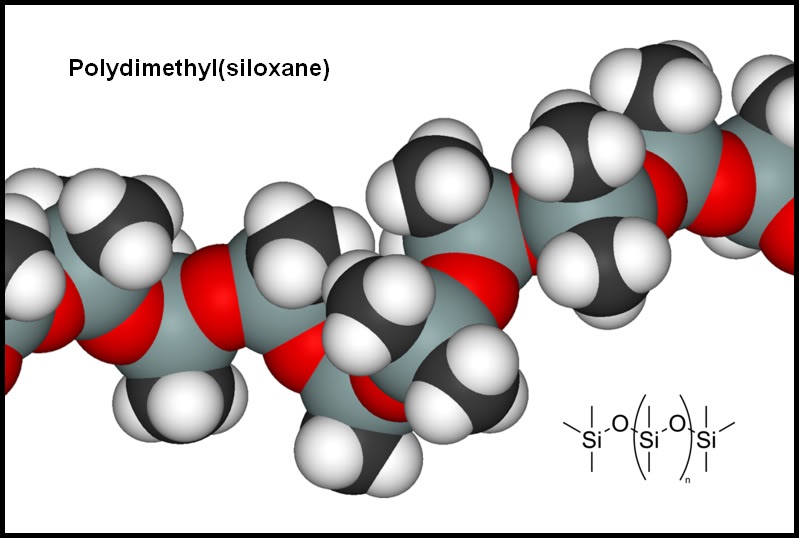
Figure 4-2: Chemical structure of polydimethyl(siloxane). (Image from Wikimedia Commons: http://en.wikipedia.org/wiki/Image:Silicone-3D-vdW.png.)
Shortly after the publication of Klystra’s pioneering work Leland C. Clark began looking for more suitable liquid breathing media. Cark’s initial efforts focused on using polyunsaturated vegetable oils such as corn and safflower oil. These oils proved injurious to lungs and Clark next evaluated the organosilanes octamethyltrisiloxane, dodecamethylpentasiloxane, decamethyltetrasiloxane, polydimethylcyclosiloxane, and polydimethylsiloxane. These compounds, commonly referred to as ‘silicone oils,’ were manufactured by the Dow Chemical Co. of Midland, MI in various chain lengths, and thus vapor pressures and physiochemical properties.[364] The organosilanes are made from a Si-O backbone to which a variety of organic groups are attached to the silicon atoms via a Si-C bond. Polydimethylsiloxane is the most common of the commercially produced organosilanes and is a polymer with a backbone consisting of a repetition of the (CH3)2SiO unit (see Figure 4-2, above). The organosilanes proved less toxic than vegetable oils, and better able to dissolve O2 and CO2, but were still too toxic to be used for liquid ventilation.
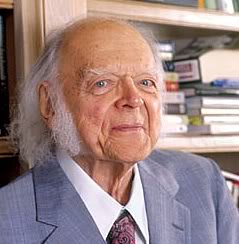
The problem of an inert and non-injurious breathing medium capable of carrying enough dissolved O2 to support life under normobaric conditions was finally solved by Leland C. Clark and Frank Gollin in 1966 with their report that a variety of fluorocarbons performed well as liquid breathing media without apparent injury to the lungs and with long-term survival of the animals.[163]
Figure 4-3: Dr. Leland C. Clark, Jr., 1918–2005 (Photo courtesy of Richard Bindstadt – Blackstar)
The PFC identified by Clark and Gollin, a ~50/50 mixture of isomers of F-alkylfurans (FC75), was evaluated under conditions of spontaneous respiration with the animals submerged in the liquid.[309] As proved the case with aqueous solutions, the PFCs delivered adequate amounts of O2, but failed to allow for effective clearance of CO2 resulting in lethal hypercarbia and acidosis. The vastly greater density and viscosity of PFCs relative to air or other gases limited the diffusion of CO2 into the liquid. An added problem contributing to the hypercarbia observed in liquid ventilation was the vastly greater work of breathing (WOB) imposed by a liquid 1,000 times as dense as air and the increased time for exhalation in the absence of active (negative pressure) pumping of the PFC from the lungs.
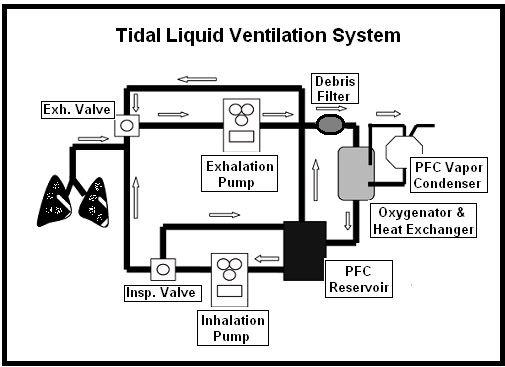
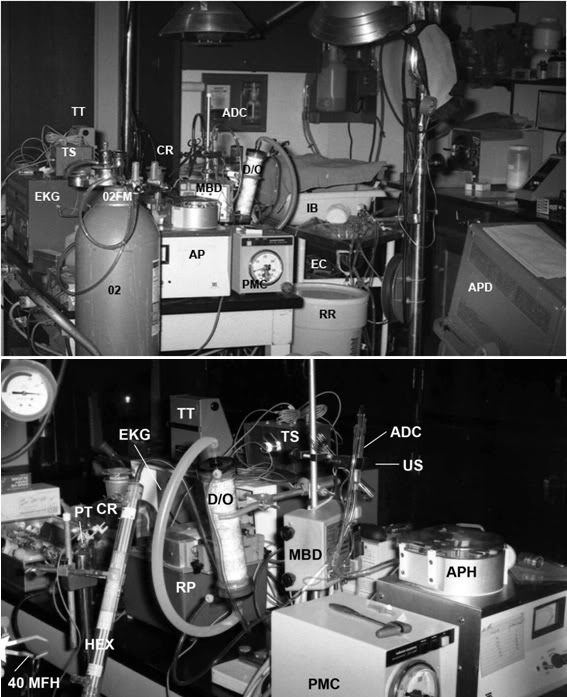
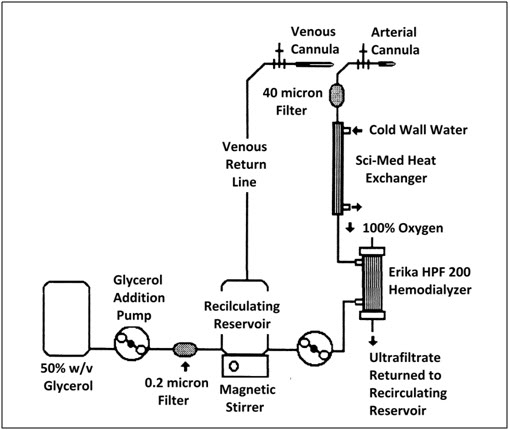
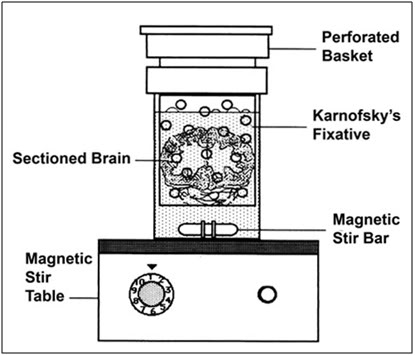
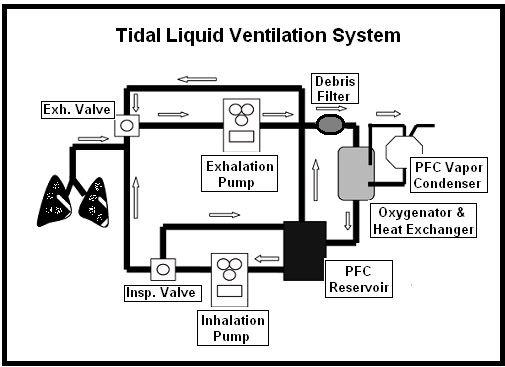
Figure 4-4: Archetypical tidal liquid ventilation (TLV) system. PFC completely replaces gas in the lungs and is moved in and out of the lungs using mechanical (usually roller) pumps. After exhalation the PFC is passed through a filter, and then through an oxygenator-heat exchanger to be scrubbed of CO2, oxygenated and warmed to body temperature before being re-infused into the lungs.
In 1970 Gordon D. Moskowitz and Thomas H. Shaffer (Figure 4-5) began work on a mechanical liquid ventilator (Figure 4-4) to overcome the problem of the increased inspiratory workload accompanying liquid breathing.[365] During the next 5-years these investigators developed progressively more sophisticated demand-regulated liquid ventilators which also began to address the need for assisted exhalation. [366],[367],[368] During the 1980s development of a variety of tidal liquid ventilators was undertaken by Shaffer, et al., and applied to animals ranging from cats [300] to preterm and neonatal lambs [369], culminating in the first clinical application of tidal liquid ventilation (TLV) to human neonates in 1989.[370]

Figure 4-5: Dr. Thomas H. Shaffer, MSE, PhD. (Photo Courtesy of Dr. Thomas Shaffer.)
Partial Liquid Ventilation (PLV)
From the beginning of liquid ventilation research with the work of Klystra in 1960, and continuing until the publication of the work of Furhman, et al. in 1991, only one kind of liquid ventilation existed; tidal or total liquid ventilation (TLV). As early as 1976 Shaffer, et al., had noticed that peak airway pressures were dramatically improved in pre-term lambs after they were returned to gas ventilation following 20 minutes of TLV.[368] The observation that lung mechanics and gas exchange remained transiently improved following TLV was extended by Shaffer, et al., in 1983 with the observations that pulmonary compliance and paO2 were increased and paCO2 was decreased during conventional gas ventilation following TLV to values lower than those that could be achieved during TLV.[300]
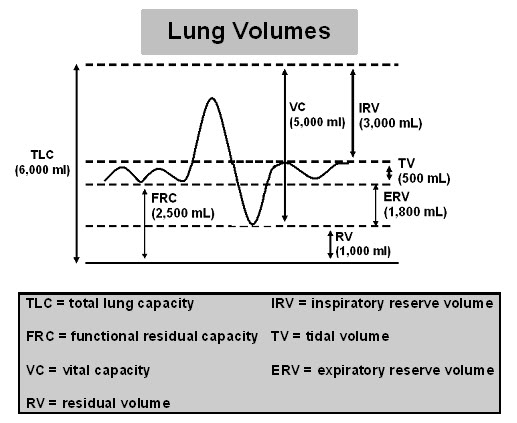
Bradley Furhman, an anesthesiologist and critical care physician at the University of Pittsburgh Medical School, noticed the enduring salutary effects of PLV following reinstitution of conventional gas ventilation in a model of infant respiratory distress syndrome (IRDS) using pre-term lambs, and he further noted that Shaffer, et al., had reported that these improvements in lung function did not occur following TLV in the healthy lung.[371] Furhman hypothesized that these salutary effects of TLV might be due to possible surfactant-like and alveolar recruitment effects of the comparatively large amounts of PFC retained in the lungs following TLV, since it was well documented that even with aggressive efforts to remove PFC following TLV, a volume approximately equal to the animal’s functional residual capacity (FRC) of 30 ml/kg remained in the lungs until it was eventually eliminated by evaporation.[370]
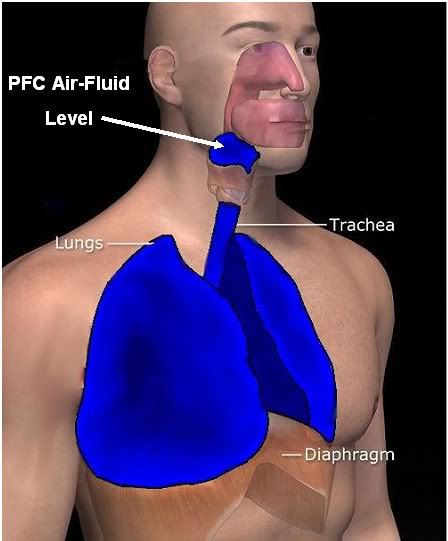
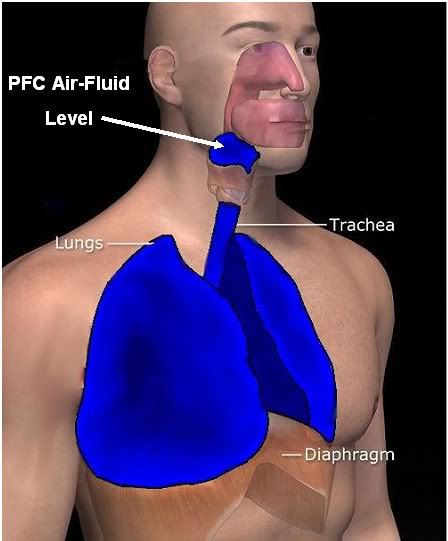
Figure 4-6: When filled to Functional Residual Capacity (FRC) the PFC forms a meniscus in the endotracheal tube. As shown at left, FRC constitutes all the volume in the lungs and trachea at the end of exhalation. (Modified by the author from the original art at Wikimedia Commons: http://en.wikipedia.org/wiki/Image:3DScience_respiratory_labeled.jpg.)
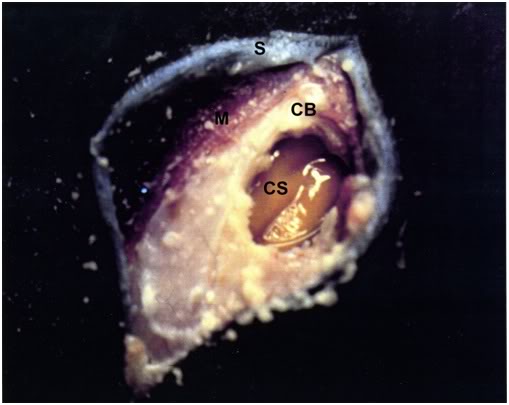
Furhman, et al., tested this hypothesis by administering FC-77 (a perfluorinated butyl-tetrahydrofuran isomer mixture) via the endotracheal tube in a volume equal to the FRC of neonatal swine.[372] As opposed to using TLV, conventional positive PPV was continued using the same parameters employed before the PFC was instilled into the lungs (Figure 4-6). This technique, christened partial liquid ventilation (PLV), proved as effective, or more effective, than TLV in decreasing airway resistance, as well as peak and mean airway pressures. PLV also seemingly abolished the need for PEEP in healthy lungs, while providing adequate gas exchange. This study not only established the effectiveness of PLV, it also posited (correctly) the mechanisms by which PLV was achieving restoration of gas exchange, increasing pulmonary compliance, and homogenizing ventilation in the lungs thus greatly reducing volutrauma (Figure 4-7, below).
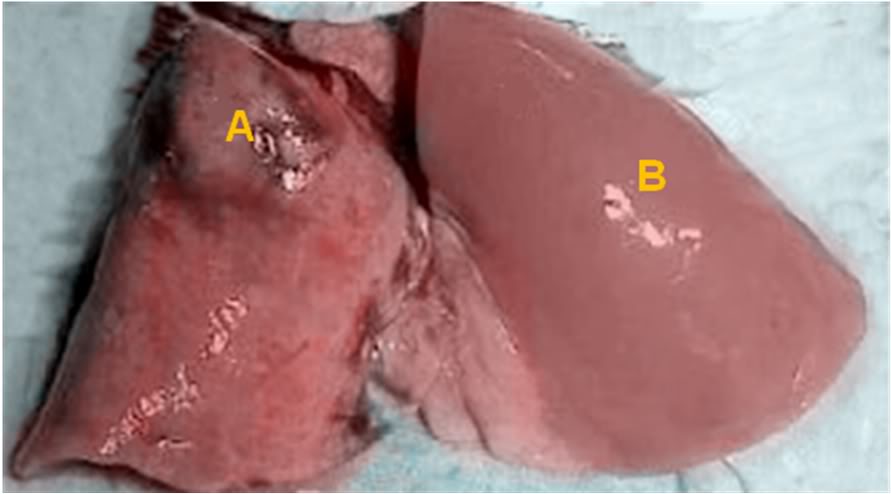
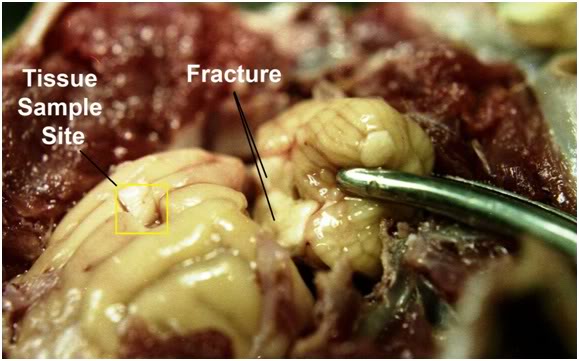
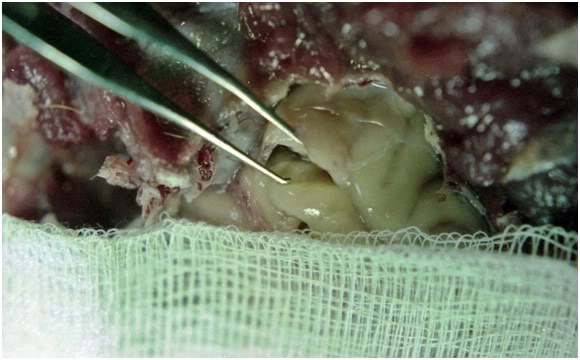
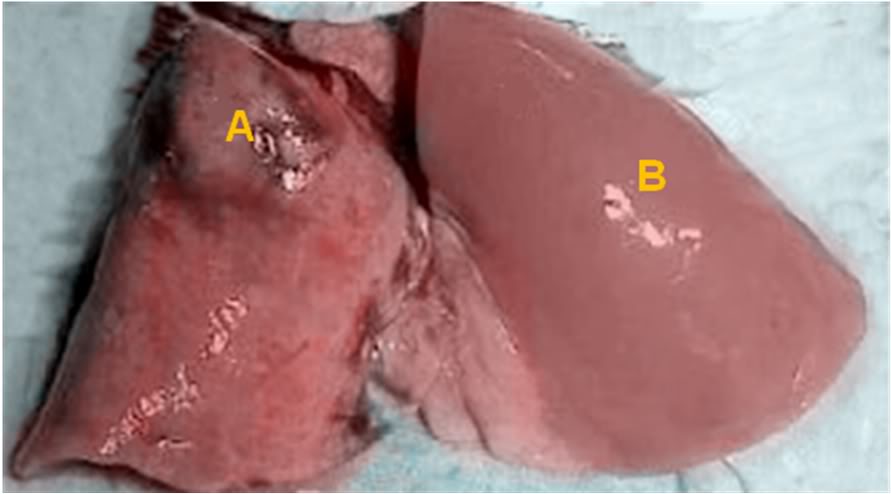
Figure 4-7: Lungs from two rabbits subjected to a model of ischemia-reperfusion injury. The lung on the left (A) shows severe volutrauma to the upper lobe (‘baby lung’) with obvious consolidation in the ventral, dependent areas of the lung. The lung on the right (B) is from an animal treated with PLV and shows no evidence of injury and is homogenously ventilated with PFC and gas. Note that the letter A has been placed on an apical ‘baby lung.’
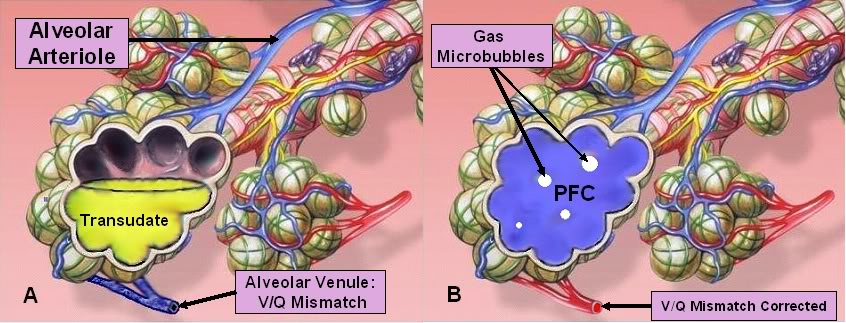
The investigators noted that due to its higher density than water the PFC rapidly flowed to the most dependent areas of the lungs and in so doing it filled collapsed alveoli and displaced serous transudate in flooded alveoli (Figure 4-9, below). With each gas breath, liquid from the large and medium caliber airways was admixed with ventilating O2 under conditions of turbulent flow, thus oxygenating it and washing it of CO2. During exhalation some, but not all of the PFC in the alveoli, flowed out into the larger airways where it was also admixed with both ventilating gas and already oxygenated PFC. During the next inspiration the alveoli were refilled with PFC that was oxygenated and cleansed of CO2. Because PFC is retained in the lungs to FRC, and gas is present in the alveoli only as micro-bubbles, if at all, the alveoli never completely empty and thus are vastly more compliant to re-inflation. As Furhman, et al., noted, the alveoli of the lungs appear to be ventilated almost exclusively with PFC throughout the ventilatory cycle with direct gas admixing occurring mostly in the larger airways (trachea, bronchi and bronchioles). Gas exchange between the blood and PFC most likely occurs due to direct PFC-alveolar membrane contact.
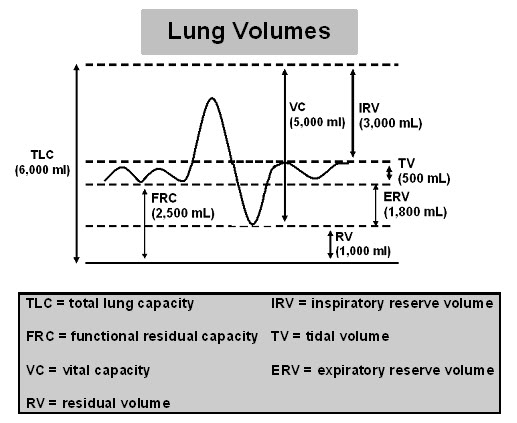
Figure 4-8: Lung volumes.
In addition to recruiting alveoli to liquid-mediated gas exchange, PLV also displaces alveolar transudate, mucus, and cellular debris by continuously lavaging the airways; macroscopic to microscopic.[373] PLV is cytoprotective of Type II alveolar epithelial cells, decreases PMNL adhesion in pulmonary capillaries [326], reduces alveolar hemorrhage, and generally preserves alveolar ultrastructure in the setting of ALI [324] and ARDS.[326]
Also of great importance is that PLV is simple to implement; it does not require novel, complex tidal liquid ventilators with an oxygenator, heat exchanger, water trap and filters – all under complex computer control. Because there is no bulk movement of PFC over long distances of airways, the resistance to PFC flow is greatly reduced, effectively eliminating the constraint of only 5 to 7 breaths per minute in TLV.[374] Because the transit times and distances between the alveoli and the bronchioles are very small in PLV (where ventilation gas admixing and gas exchange is occurring) and because CO2 is probably exchanged in micro-bubbles in the PFC which are far smaller than would be the case in a ‘sphere’ of PFC the diameter of the alveolus (~250µ), the problem of hypercarbia is also eliminated.[375]
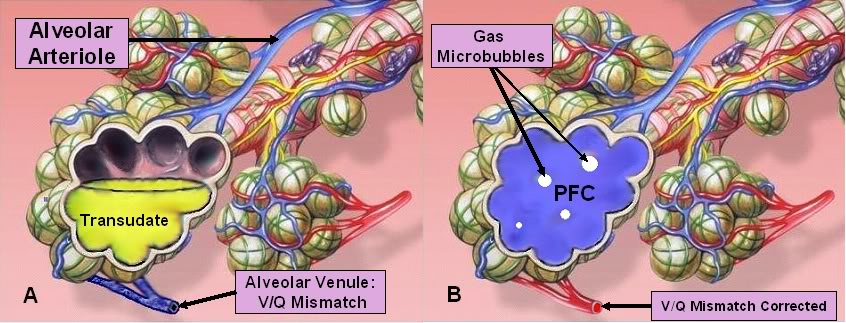
Figure 4-9: A: Alveoli are flooded alveoli in ARDS or pulmonary edema. When PFC is, literally, poured down the endotracheal tube it flows under gravity (due to its ~1.8x density of water) to the most dependent areas of the lungs. B: In so doing it opens the collapsed alveoli and displaces edema fluid from them. (Modified from original art by Patrick J. Lynch, medical illustrator, and is from Wikimedia Commons.)
From 1991 to 2000, PLV was extensively investigated in a number of different animals employing a variety of models of lung injury; saline FTLV, oleic acid injury, smoke inhalation, prematurity, intestinal ischemia, lung transplantation injury, and pneumococcal pneumonia.[376], [377], [378],[379],[380],[381] These studies, with no notable exceptions, showed marked benefit for PLV in ALI and ARDS.
In 1993 Leach, et al., [164] carried out the first clinical trial of PLV in IRDS (Figure 4-10). This was followed by a number of clinical trials for ARDS in both children [382] and adults.[383] These trials were sponsored by Alliance Pharmaceuticals, Inc. of San Diego, CA (Alliance) in an effort to obtain FDA approval for the use of Perflubron™ as the first gas exchange PFC in PLV.
In 2006, after 5 years of delay, the ‘definitive,’ Phase III, prospective, randomized clinical trial (RCT) of PLV in ARDS was published (LiquiVent™ study).[384] For reasons that are only now being understood, this trial showed PLV (using Perflubron™ at a dose equal to FRC (30 ml/kg), and at a lower dose of 10 ml/kg, to yield a worse outcome than conventional PPV with increased overall mortality and increased days requiring mechanical ventilation: The 28-day mortality in the control group was 15%, versus 26.3% in the low-dose (p=0.06) and 19.1% in the high-dose (p = 0.39) PLV groups. There were more ventilator-free days in the control group (13.0 ± 9.3) compared with both the low-dose (7.4 ± 8.5; p=0.001) and high-dose (9.9 ± 9.1; p =0.043) groups. Most remarkably, there was a high incidence of barotrauma: 34% pneumothoraces in the phase II LiquiVent™ trial (20% in the control group) and 29% and 28% in the phase III LiquiVent™ trial (control, 9%). Pneumothoraces requiring the placement of chest tubes is an ominous complication of PPV in ALI and ARDS and is associated with increased mortality, duration of ventilator time and length of stay in the ICU. In view of the consistently diverse, positive and well conducted animal studies demonstrating unequivocal benefit, this result was surprising.

Figure 4-10: Initiation of PLV in a neonate with IRDS. The only novel piece of equipment used was a luer-loc one-valve interposed between the endotracheal tube and the 16 mm connector to the ventilator to facilitate intra-tracheal administration of Perflubron™ without having to disconnect the patient from the breathing circuit. (Photo courtesy of Alliance Pharmaceutical, Inc.)
The reasons for the failure of the Phase III LiquiVent ™ RCT are both complicated and subtle – and are still being debated today. [385] The likely reasons for the failure of the Phase III study have important implications, not only for the future of PLV in ALI and ARDS, but also for the optimum use of PLV and LAPC in emergency and critical care medicine. The reasons for PLV’s failure are rooted in difficulties and errors that have plagued translational research from animals to humans in many areas of medical research.[386] What follows is a point-by-point evaluation of the possible causes of failure of the Phase III PLV trial as well as an analysis of the implications of these problems for LAPC.
Unanticipated Effect of Lung Protective Ventilation Strategies
The Phase III trial was designed in 1997, begun in 1998, and completed in 2002. This was well before the first report of the efficacy of lung-protective ventilation in reducing mortality in ARDS and ALI was reported in 2000 [387] and 7 years before the first influential ARDSnet study was published.[388] The criticality of minimizing barotrauma and volutrauma, even over maintaining gas exchange at optimum physiological levels, was thus not taken into consideration in the LiquiVent™ study design. This was especially significant because, due to subtle shortcomings in the design of most of the animal studies, it was not understood that PLV is a source of barotrauma and volutrauma; even when far less than full FRC-dosing is used under circumstances most like those encountered clinically (see ‘Failure to Establish a Dose-Response Curve,’ below).
While the LiquiVent™ study experimental group had a worse outcome than the control group, it should be noted that the absolute results were actually no better (or worse) than those reported in the previously cited ARDSnet studies validating lung protective ventilation (i.e., 15 to 26%). This is especially worth noting because all 3 groups of the LiquiVent™ study patients were considerably sicker than the patients in the ARDSnet studies. The objective entry criteria for the LiquiVent™ study were an initial PaO2/FiO2 <200mmHg followed by a failed (PaO2/FiO2 < 300 mmHg) response to a PEEP of ≥ 13 cm H2O at a FiO2 ≥ 0.5. By contrast, the ARDSnet patients only needed to have a PaO2/FiO2 of < 300 mmHg with no requirements for PEEP or FiO2 upon randomization. One possible reason for the superior outcome in the LiquiVent™ control group, compared to that seen in most other studies of ARDS at that time, is that Alliance selected only the very best centers of excellence in the management of ALI and ARDS to conduct the trials. By contrast, ARDSnet studies were also conducted on a contract basis by NIH at institutions that were more representative of the actual quality of care available at large metropolitan hospitals in the U.S. Alliance thus placed LiquiVent™, and consequently the entire field of PLV, on trial in a setting with the sickest patients receiving the best medical management for ARDS
Defective Translational Research Models
The animal models of ALI and ARDS used to evaluate PLV did not model the real-world course of lung injury in clinical illness. Researchers typically inflict an insult and then wait a uniform, and often unrealistically short time, for the injury to develop. By the time human patients in respiratory distress enter the ICU they have usually been ill for many hours, or even days, and as a consequence the degree of pulmonary compromise, and in particular, pulmonary edema, may be greater. Furthermore, animal models of lung injury are inherently more homogenous than is usually the case in human ARDS. Heterogeneity of injury is one of the hallmarks of both ALI and ARDS in humans, and heterogeneity means that normal or minimally injured areas of lung will be subjected to the same conditions as more severely injured areas (see discussion of varying requirements for PEEP depending upon the degree of injury individual alveoli under the heading, ‘The PFC Air Interface and Shear Effects in the Small Airways,’ below).
These observations have other important implications because loading to the theoretical FRC (30 ml/kg) in ill and often aged humans may not be possible, in the sense that the ‘normal’ or predicted volume of lung to be recruited may not be available. Alveoli can be filled with PFC only if there is enough room in the thorax to allow them to fill. If fluid in severely edematous lung parenchyma stubbornly resists relocation to the vascular compartment due to hypoalbuminemia and an interstitial pressure in excess of the hydrostatic force generated by the PFC, or if for other mechanical reasons there is not sufficient volume to accommodate a FRC-dose of PFC, then the result will be volutrauma and barotrauma to the less dependent lung. This possibility was noted by Cox, et al., as early as 1997 and was later raised in a study done by Lim et al., in 2000.[389]
Failure to Establish a Dose-Response Curve
While as previously noted, a wide range of animal models, and models of injury were investigated with respect to PLV, there was little study to determine the optimum dose-response curve of either LiquiVent™ or other PFCs used in PLV. In hindsight this seems strange because in the experimental evaluation of any novel drug the first step is usually to establish a dose-response curve and thus to bound the ‘safe and effective dose.’ This was not done in PLV and those studies which documented injury from PLV in normal lungs at FRC dosing were arguably not given the attention they deserved.[390],[391]
Recently, the work of Dreyfuss and Ricard [392] has demonstrated that dosing to FRC in healthy rats actually causes alveolar capillary leak and induces lung injury. In a series of elegant studies they have examined the complex relationship between PFC dose, PEEP and Pplat. Their studies indicate that the probable ideal dose of PFC (or of Perflubron™ in this case) is ~ 3 ml/kg; 10% of FRC, and still only 30% of the 10 ml/kg dose used in the ‘low dose’ LiquiVent™ study.[393] Furthermore, these investigators have documented that FRC dosing with Perflubron™ causes gas trapping in the lungs, and that under these circumstances, paradoxically, PEEP is protective.[391]
Gas Trapping and Selection of the Appropriate PFC
Perflubron’s™ comparatively low vapor pressure is similar to that of perflurodecalin and thus probably results in a lower spreading coefficient relative to most other PFCs used in the animal studies. This would likely result in slower dynamic flow during inspiration and in ‘plugging’ of medium caliber airways (with the previously noted effect of gas-trapping) due to high gas-fluid interfacial tension.[394],[395] These effects may contribute to barotrauma and volutrauma when Perflubron™ is administered to full FRC.[396],[397]
It now appears that if PLV is to have any chance at conventional clinical application in the West, clinical trials will have to start from scratch, quite possibly with a different PFC, or blend of PFCs, being used to achieve the pharmaco-physical properties required for the particular application – including possibly tailoring the medium to the size of the patient’s intermediate sized airways (which are greatly different between neonates, children and adults) and to the particular application at hand. For instance, as Jeng, et al., (from Schaffer’s group) states:
“In terms of clinical application, the appropriate fluid for liquid assisted ventilation will depend on the clinical situation. For example, a more viscous fluid may be more appropriate for supporting the lung during extracorporeal membrane oxygenation during which the PFC application is aimed at preventing atelectasis and fluid flux across lung-at-rest conditions. In contrast, a less viscous fluid may be preferred for TLV during which tidal volumes of fluid are exchanged. For PLV, a fluid with low vapor pressure would reduce dosing requirements during the course of the treatment. Thus, the data presented herein further relate fluid physical properties with liquid ventilation applications.”[304]
The PFC Air Interface and Shear Effects in Small Airways
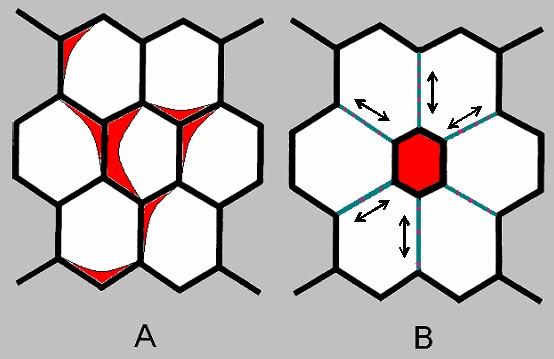
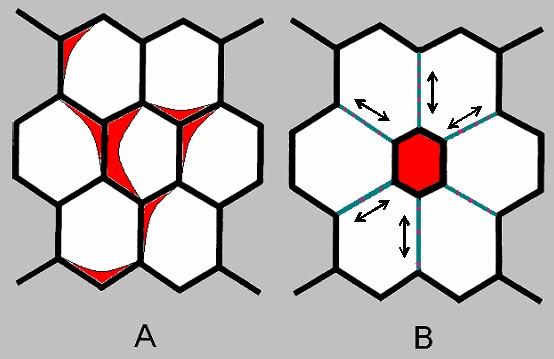
Figure 4-11: The shear- inducing effect of a single flooded alveolus on neighboring alveoli. Open alveoli (A) expand evenly in unison and experience no shear. After alveolar flooding and collapse (B) shear forces occur on the adjoining alveolar septa. PFC filled; partially filled and unfilled alveoli and other acinar structures will be subject to the same damaging shear forces as is the case when aqueous media are present in the acini.
Although the alveolar air-liquid interface is eliminated during PLV, giving PLV its PEEP and surfactant-like properties, a PFC-gas interface is created. The law of Laplace ( P = 2γ/r) describes the relationship between the pressure to stabilize an alveolus (P) and surface tension at the gas-PFC interface of an alveolus (γ) in relation to the radius of the alveolus r. [398] In the normal lung, surfactant present at the gas-liquid interface lowers the air-liquid surface tension in lockstep with decreasing alveolar radius (to nearly 0 mN · m-1 for low alveolar radii), thus keeping the ratio of γ/r of the alveolus constant and guaranteeing alveolar end expiratory stability at low pressures.[399],[400] By contrast, PFCs exhibit a constant gas-PFC surface tension for any alveolar radius. This means that at the end of exhalation, the alveolar radius will be quite small, while the surface tension remains unchanged, and therefore very high compared to when the alveolus is inflated. Thus, the alveoli will collapse unless they are supported by PEEP from the ventilating gas.[401] The implication is that PFC-derived ‘liquid PEEP’ must always be balanced by precisely the right amount of ‘gas PEEP’ to prevent end-expiratory collapse of non-PFC-filled alveoli (Figure 4-11). This presents a formidable challenge in both the laboratory and the clinic.
Partial Liquid Ventilation and the Law of Laplace
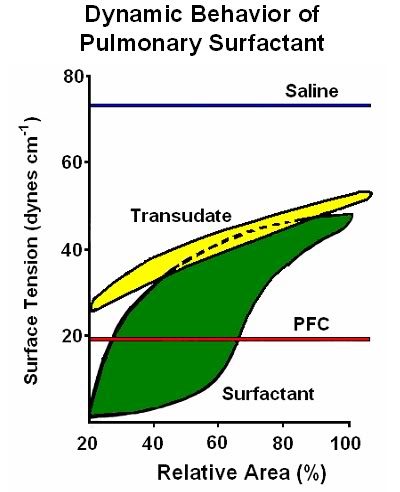
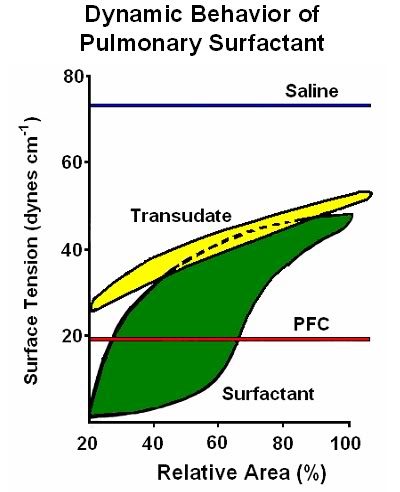
Figure 4-12: In attempting to determine the extent to which PFC is likely to cause alveolar injury due to gas-liquid mediated shear forces, and variable distention of alveoli filled with PFC as opposed to gas, it is instructive to compare the dynamic behavior of PFC (red line) with surfactant (green) as well as with other liquids, such as pulmonary edema transudate (yellow) (which contains dissolved surfactant), and saline (blue line). While PFC exerts far less surface tension than saline, it still exerts a force at the air-PFC interface of ~20 dynes cm-1, and, like saline, lacks the dynamic responsiveness to changes in surface area which are the unique property of surfactant and surfactant containing solutions.
In addition to the problem of end-tidal alveolar collapse, high shear forces at the alveolar membrane as a result of insufficient PEEP during PLV may cause alveolar rupture and consequently gas/PFC leak and the development of pneumo- and/or perflurothorces.[402] The complexity and difficulty of this problem becomes clearer when consideration is given to the fact that the amount of ventilator-applied ‘gas PEEP’ will be a function of the pathological condition of each alveolus (which will vary widely in the same lung, let alone from patient to patient). This is so because the presence of a thin film of PFC in the alveolus will only be beneficial in alveoli where the native surfactant has failed to maintain alveolar patency (diameter).
In those compromised alveoli that are unable to reduce surface tension to the gas-PFC interfacial tension, the level of ‘gas PEEP’ required to keep them open at the end of exhalation will be lower during PLV than the level of ‘gas PEEP’ during conventional mechanical ventilation. Conversely, in alveoli with functioning surfactant, (i.e., able to reduce their surface tension to below that of the gas-PFC interface) there will be an interaction between PFC and the normal alveolar membrane fluid, leading to levels of ‘gas PEEP’ with PLV higher than those required to keep the alveoli open with ‘gas PEEP’ required in conventional ventilation alone (Figure 4-12). In the clinical milieu this implies careful titration of PFC dose during initiation and maintenance of PLV and equally careful titration of PFC ‘removal’ (i.e. evaporation) or weaning from PFC during the transition from PLV to gas-only PPV.[401]
Even assuming that the means can be developed to determine and control these parameters, the seemingly intractable problem of inhomogeneous gas distribution during tidal gas ventilation in PLV remains. Gas will go preferentially to the least PFC liquid loaded and least dependent airways and this will likely produce over-distension and volutrauma much as happens in the edematous consolidated lung. At a minimum it will be necessary combine fluid PEEP with pressure-controlled ventilation in a way such that the pressure in any alveolus does not exceed the pressure of the ventilating gas.[381] Failure to prevent shear or alveolar hyperinflation will result not only in direct mechanical injury to the alveolar membrane and pulmonary capillaries, [403] but also in both local and systemic injury from pro-inflammatory cytokines whose release by alveolar epithelial cells is triggered by even modest shear stress or over-distension.[404],[405]
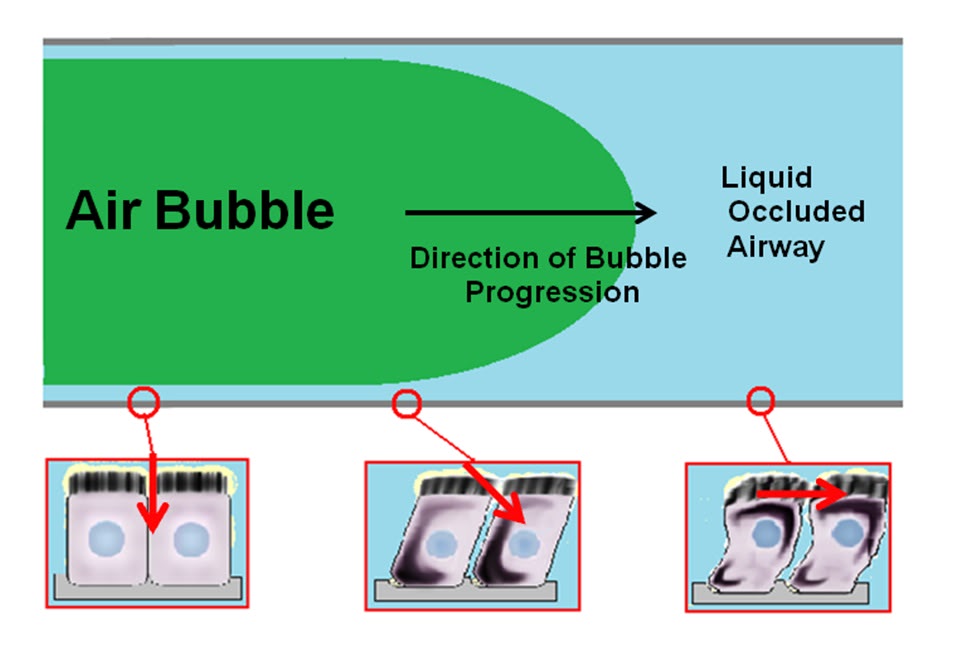
An additional source of shear injury in PLV and thus presumably LAPC is only now beginning to emerge. Research on VLI has predominately focused on the role of high inflation pressures and large tidal volumes.[404],[406],[407] However, ventilation at low lung volumes and pressures results in a different type of lung injury, in which airway instability leads to repetitive collapse and reopening of the terminal airways.[408] This type of injury is relevant to LAPC and PLV because the air-PFC interface behaves similarly to the cyclically re-inflated collapsed airway. During reopening of collapsed airways a finger of air moves through the airway generating stresses on airway walls and injuring the airway epithelium.[409],[410],[411],[412] This does not occur during normal tidal ventilation because pulmonary surfactant stabilizes the airways and prevents their collapse during exhalation.
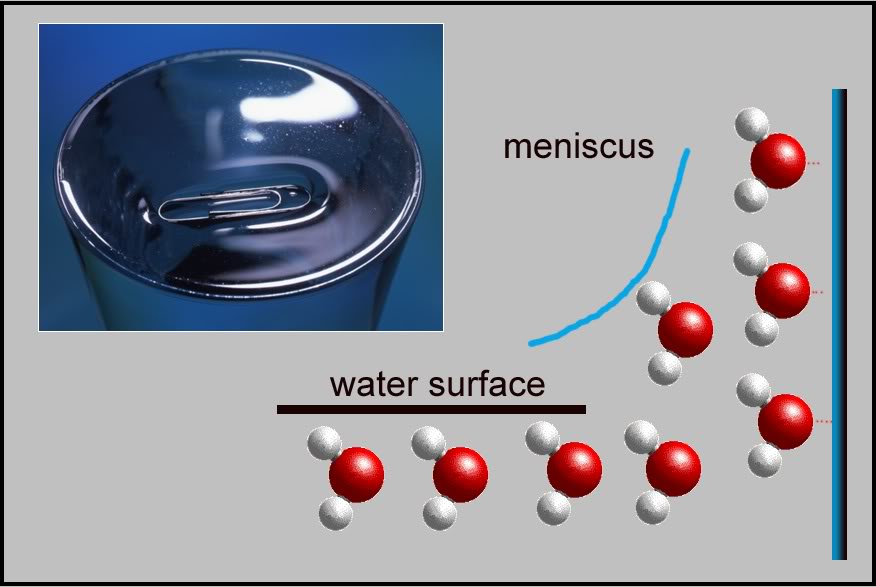
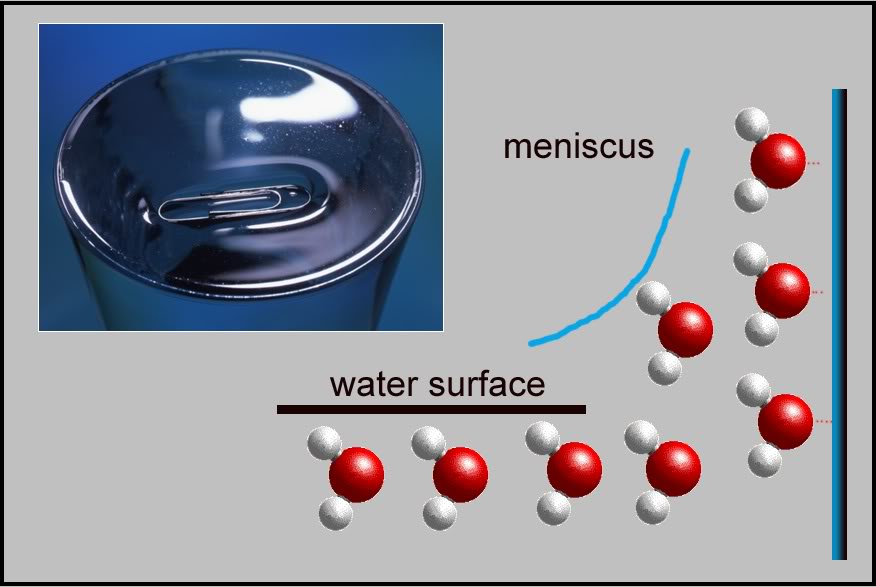
Figure 4-13: The power of surface tension is perhaps most easily illustrated by meniscus formation at tripartite air-cylinder-liquid interface. When water wets a small diameter tube the liquid surface inside the tube forms a concave meniscus, which is a virtually spherical surface having the same radius, r, as the inside of the tube. The tube experiences a downward force of magnitude 2πrdσ.The gas-liquid interface under the influence of the tidal forces of ventilation generates enormous shear stress on the respiratory epithelium of small caliber airways. The ‘pull’ exerted by PFC on a capillary wall is approximately 1/5th that of saline, or ~ 0.4 πrdσ; more than enough to cause endothelial cell injury during tidal ventilation. A metal paperclip floating atop a glass of water illustrates the power of surface tension.
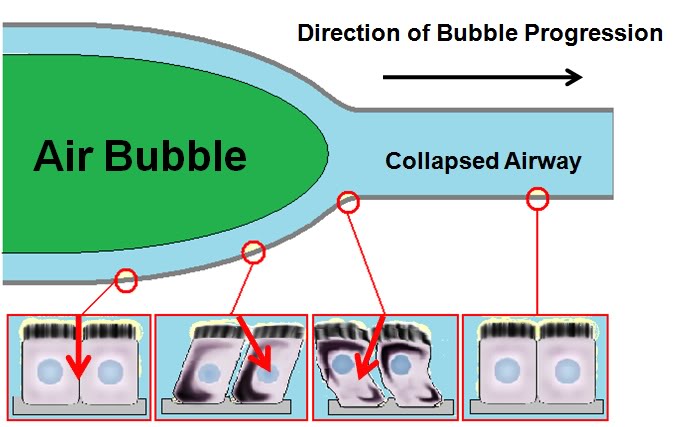
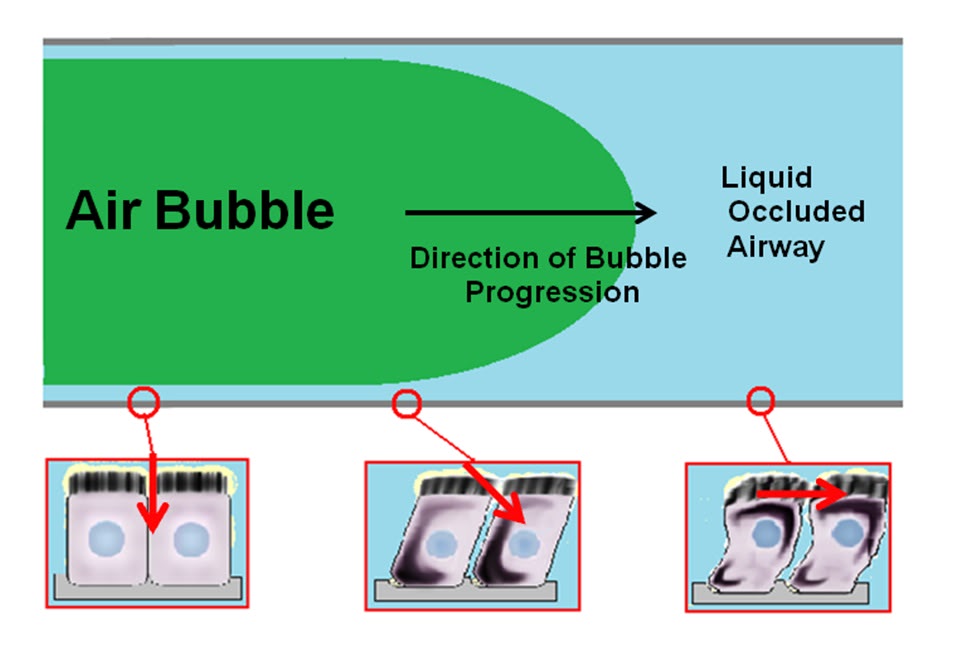
However, in ARDS, and where bulk liquid mixed with gas is present in the small airways (including PFC) surfactant cannot act to protect the airway epithelium against the stress field exerted on the walls of these airways as bubbles move to and fro through the liquid inside them. Bilek, et al., have investigated this phenomenon in vitro and have modelled it computationally as a semi-infinite bubble progressing through a compliantly collapsed airway, as well as a bubble progressing through a rigid tube occluded by fluid. [413] In this process, the airway walls are separated in a peeling motion as the bubble traverses the airway. This effect has been indirectly documented by experimental observation in vivo. [414],[415] Airway reopening induces large and rapid changes in normal and shear stress along the airway walls. These spatial and temporal gradients of stress exert dynamic, large, and potentially damaging stresses on the airway epithelium that do not occur under one-phase steady-flow conditions.[411], [416],[415] These forces are shown schematically in Figure 4-14. The shear stresses induced by bubble progression along both collapsed and liquid filled airways cause direct trauma due to substrate stretch-induced injuries of pulmonary epithelial cells as a result of stretching of the plasma membrane causing small tears.[417],[404] Additionally, mechanical stresses from the fluid flow may stretch the plasma membrane either directly, or as a consequence of cellular deformation.
For a low profile, predominately flat region of a cell, the non-uniformly distributed load may regionally deform the membrane. In addition, the normal-stress difference could induce transient internal flows within the cell that exert hydrodynamic stresses on the intracellular surface of the cell membrane, which might injure the membrane by the same mechanisms as extracellular stresses, and additionally be disruptive to the cytoskeleton. Bilek, et al., also describe the effects of irregular airway topology on forces generated at the air-liquid interface. They note that bulges of as little as 2 μ into the lumen of an airway result in greatly amplified shear stresses. Such bulges are commonplace in healthy airway epithelium as a result of the protrusion of epithelial cell nuclei into the airway lumen. The smoothness of the pulmonary epithelium is greatly compromised in ARDS and pulmonary edema and this may be expected to exacerbate topologically mediated shear injury to the small airways. It is interesting to note that Bilek, et al., found that the addition of surfactant to their model systems abolished shear injury in both reopening and bubble- traversing, saline occluded models; perhaps as a result of moderating liquid film thickness over the surface of the airway epithelium thereby decreasing the flow resistance and stress amplification. To what extent this may be applicable in the setting of PLV or LAPC using PFCs is unclear, since presumably surfactant is only effective by being dissolved in the bulk liquid present in the airways (i.e., in the Bilkek, et al., model, saline).
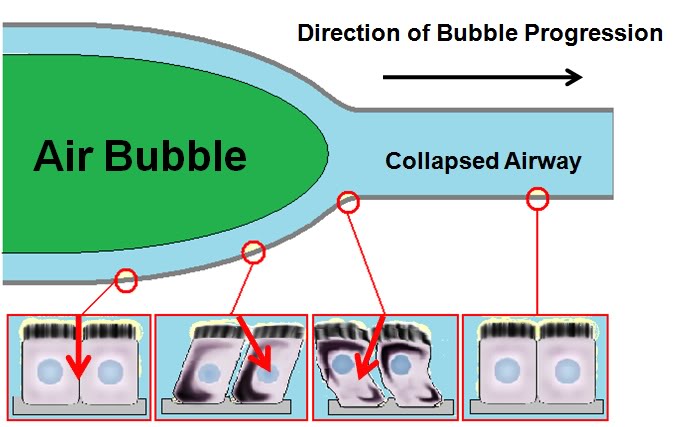
Figure 4-14: Hypothetical stresses imparted on the epithelial cells of an airway during reopening. A: a collapsed compliant airway is forced open by a finger of air moving from left to right. A dynamic wave of stresses is imparted on the airway tissues as the bubble progresses. Circles show the cycle of stresses that an airway epithelial cell might experience during reopening. The cell far downstream is nominally stressed. As the bubble approaches, the cell is pulled up and toward the bubble. As the bubble passes, the cell is pushed away from the bubble. After the bubble has passed, the cell is pushed outward.
B: A fluid ‘occlusion’ in a rigid narrow channel is cleared by the progression of a finger of air moving from left to right. A dynamic wave of stresses is imparted on the pulmonary epithelial cells lining the channel wall. The circles show the cycle of stresses that the cells might experience during reopening. Far downstream, the cell is pushed forward and slightly out. As the bubble approaches, a sudden rise in pressure and a peak in shear stress occurs, pushing the cell forward and outward with much greater force. After the bubble has passed, the cell is pushed outward. Pressure gradients generated in the presence of an air-PFC interface can also be expected to create normal stress imbalances on the cell membrane over the length of the cell. (Illustration and accompanying text reproduced from Bilek, AK, Dee, KC, Gaver, DP, III. Mechanisms of surface-tension-induced epithelial cell damage in a model of pulmonary airway reopening. J Appl Physiol 94:770-783; 2003.)
These problems may only (if ever) be solved when applying PLV to ALI and ARDS by eliminating tidal gas ventilation and replacing it with high frequency oscillating ventilation (HFOV) which yields uniform and far lower mean airway and Pt pressures and abolishes peak pressures associated with inspiration [418]; although this modality did not prove superior to either PLV or HFOV alone in animal studies – albeit using high (FRC) doses of PFC.[419]
In the case of LAPC, the short duration of FTLV as compared to that required for the treatment of ARDS using PLV may not cause sufficient shear injury to be of clinical concern, particularly in the absence of extensive preexisting pulmonary pathology. In the event that shear injury does prove to be a problem, it may be possible to use HFOV in combination with a more or less continuous process of PFC introduction and removal at or near the level of the carina. Although, the extent to which HFOV would be effective in rapidly exchanging liquid, as opposed to gas, between the large and small airways is unknown.
The Best as the Enemy of the Good
Finally, another possible factor in the discrepancy between the human and animal trials of PLV was the very close control over the availability of Perflubron™ to investigators exerted by Alliance. In part, this tightly controlled and highly selective distribution of Perflubron™ to only a small number of carefully vetted researchers was driven by the high intrinsic cost of the molecule, and by the cultural and regulatory milieu currently present in the West. Gone are the days when pharmaceutical companies freely distributed putative new drugs for studies more or less upon request. The staggering cost of regulatory approval for a new drug, coupled with often irresponsible ‘research’ aimed at inciting the media frenzy that occurs whenever the toxicity or carcinogenicity of any novel or synthetic molecule (the so-called ‘cyclamate-effect’) is newly demonstrated (regardless of the lack of soundness of the experimental design), has understandably made drug developers cautious about to whom they entrust the evaluation of potentially multibillion dollar compounds. An unfortunate effect of this abundance of caution is that novel drugs are often protected from robust evaluation under more widely varying conditions that more closely approximated those seen in the real world.
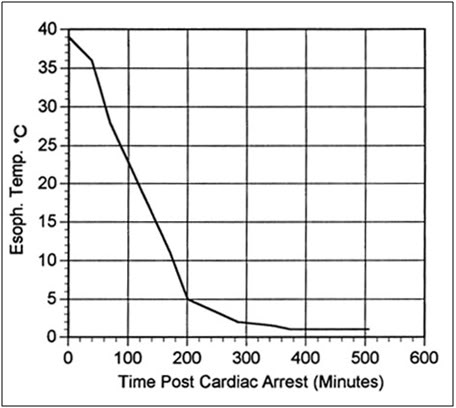
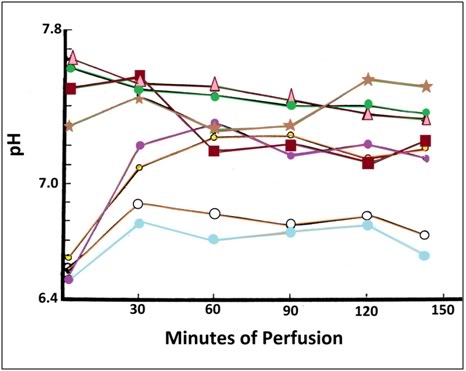
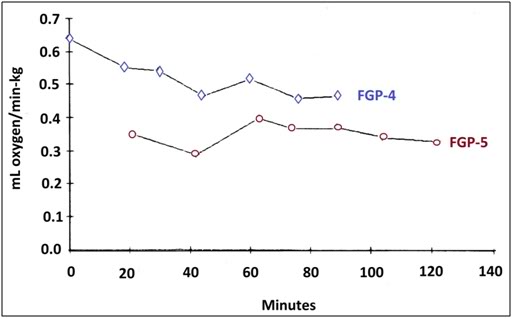
Implications for SCA and LAPC
To a much greater degree than was the case with the LiquiVent™ trials (and PLV studies in general), the study being used to initially determine the feasibility of LAPC for SCA using a TLV-type approach conducted by the author and his colleagues [272] suffers from the same defects that plagued the Alliance PLV studies. This study was conducted on healthy dogs – not on animals that were undergoing CPR with the associated very high peak and mean airway pressures. As was the case in the LiquiVent™ studies, this work preceded the ARDSnet data demonstrating the importance of low tidal volume ventilation and lung protective strategies in general, including minimizing peak and plateau airway pressures. At the time this study was published the authors were, like the LiquiVent™ investigators, unaware of the adverse effects of loading with PFC to FRC – although we certainly observed volutrauma and barotrauma – and became very sensitive to the need for controlling peak and mean airway pressures, as well as to a nuanced shaping of the flow-pressure curve. Indeed, the problem of automating the ideal flow-pressure algorithm has reportedly remained elusive, and ventilation using the technique of LAPC we reported is still least traumatically performed by hand.[420]
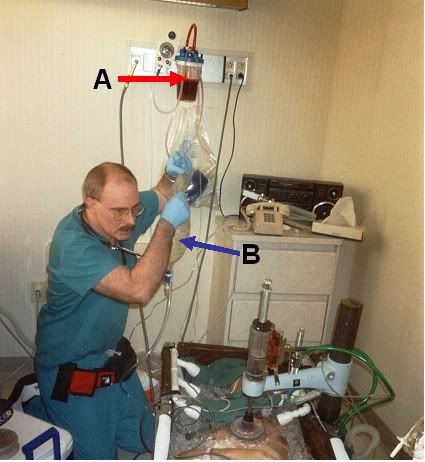
Figure 4-15 (left): The first human cryopatient, Eleanor Williams, undergoing LAPC on 02 March, 2002; several 1,500 ml FTLVs of PFC chilled to ~4ºC were administered by the author using gravity delivery from a flexible 2-liter peritoneal dialysis bag (blue arrow) and then suctioned out. This patient experienced massive hemoptysis immediately after the start of CPS and before LAPC was initiated (red arrow). The patient hemorrhaged ~1,500 ml of blood in less than 5 minutes: underscoring the catastrophic nature of pulmonary bleeds in the setting of friable lungs and CPR. (Photo courtesy of the Alcor Life Extension Foundation.)
The recent insights into the reasons for the failure of PLV Phase III clinical trials suggest that to the extent it is possible to reduce the volume of gas breaths and of the FTLVs required to facilitate heat exchange (i.e., delivery of PFC to and retrieval of PFC from the lungs on a cyclical basis) this will likely reduce the severity of lung injury resulting from LAPC. The measured intrapulmonary pressure in patients undergoing TLV in the Phase III LiquiVent™ study were ~60 cmH20 and this resulted in a high incidence of air leak. Intrathoracic pressure in CPR is typically in the same range; 45 to 55 mmHg or ~61 to 75 cmH20.[253] The combination of LAPC at FRC with CPR is unknown territory and should be approached with caution; and hopefully also approached with additional studies in animal models of extended duration CPR with long term follow up of the animals.
References
1. American-Heart-Association, Heart Disease and Stroke Statistics – 2008 Update. . 2008, American Heart Association: Dallas, Texas.
2. de Vreede-Swagemakers, J., et al., Out-of-hospital cardiac arrest in the 1990′s: a population-based study in the Maastricht area on incidence, characteristics and survival. . J Am Coll Cardiol, 1997. 30: p. 1500-5.
3. American-Heart-Association-and-National-Research-Council, Standards for cardiopulmonary resuscitation (CPR) and emergency cardiac care (ECC). . JJ Amer Med Assoc, 1974. 227(suppl): p. 833-68.
4. Sakai, A., Sudden deaths among male employees: a six-year epidemiological survey. J Cardiol, 1990. 20: p. 957-61.
5. Safranek, D., Eisenberg, MS, Larsen, MP., The epidemiology of cardiac arrest in young adults. Ann Emerg Med, 1992. 21: p. 1102-6.
6. Viskin, S., Belhassen, B., Idiopathic ventricular fibrillation. American Heart Journal, 1990. 120: p. 661 – 671.
7. Skogvoll, E., et al., Out-of-hospital cardiopulmonary resuscitation: a population-based Norwegian study of incidence and survival. . Eur J Emerg Med, 1999. 6: p. 323-30.
8. Weale, F., The efficacy of cardiac massage. Lancet, 1960. 1: p. 990-96.
9. Eisenberg, M., Cardiac Arrest and Resuscitation: A tale of 29 cities. Ann of Emer Med, 1990. 19: p. 179-86.
10. Kentsch, M., et al., Early prediction of prognosis in out-of-hospital cardiac arrest. Intensive Care Med, 1990. 16: p. 378-83.
11. Troiano, P., et al., The effect of bystander CPR on neurologic outcome in survivors of prehospital cardiac arrests. Resuscitation, 1989. 17: p. 91-8.
12. Bossaert, L., Van Hoeyweghen, R., Bystander cardiopulmonary resuscitation (CPR) in out-of-hospital cardiac arrest. The Cerebral Resuscitation Study Group. . Resuscitation, 1989. 17(Suppl): p. S55-69; discussion S199-206.
13. Stueven, H., et al. , Bystander/first responder CPR: ten years experience in a paramedic system. Ann Emerg Med, 1986. 15: p. 707-10.
14. Lombardi, G., Gallagher, J, Gennis, P., Outcome of out-of-hospital cardiac arrest in New York City. The Pre- Hospital Arrest Survival Evaluation (PHASE) Study [see comments]. JAMA, 1994. 271: p. 678-83.
15. McCarthy, M., Looking after your neighbors Seattle-style. Lancet, 1998. 351: p. 732.
16. Hayward, M., Cardiopulmonary resuscitation: are practitioners being realistic? Br J Nurs, 1999. 8: p. 810-4.
17. Bengtsson, M., A psychiatric-psychosocial investigation of patients who had survived circulatory arrest. Acta Psychiat Scan, 1969. 45: p. 327.
18. Roewer, N., Kloss, T, Puschel, K., Long-term result and quality of life following preclinical cardiopulmonary resuscitation. Anasth Intensivther Notfallmed, 1985. 20: p. 244-50.
19. de Vos, R., Quality of life after cardiopulmonary resuscitation. Resuscitation, 1997. 35: p. 231-6.
20. Phillips, S., Resuscitation for cardiogenic shock with extracorporeal membrane oxygenation systems. Semin Thorac Cardiovasc Surg, 1994. 6: p. 131-5.
21. Younger, J., et al., Extracorporeal resuscitation of cardiac arrest [see comments]. Acad Emerg Med, 1999. 6: p. 700-7.
22. Matsuwaka, R., et al., Emergency percutaneous cardiopulmonary support for patients with cardiac arrest or severe cardiogenic shock. Nippon Kyobu Geka Gakkai Zasshi, 1996. 44: p. 2006-10.
23. Myerburg, R., Clinical, electrophysiologic, and hemodynamic profiles of patients resuscitated from pre-hospital cardiac arrest. . Amer J Med, 1980. 68: p. 568.
24. Safar, P., Abramson, NS, Angelos, M, et al., Emergency cardiopulmonary bypass for resuscitation from prolonged cardiac arrest. Am J Emerg Med, 1990. 8: p. 55-67.
25. Peterson, M., et al., Outcome after cardiopulmonary resuscitation in a medical intensive care unit. Chest, 1991. 100: p. 168-74.
26. Gener, J., et al., Immediate and 1-year survival after cardiopulmonary resuscitation at an intensive care unit. Med Clin (Barc), 1989. 93: p. 445-8.
27. Rubertsson, S., et al., Blood flow and perfusion pressure during open-chest versus closed-chest cardiopulmonary resuscitation in pigs. Am J Emerg Med, 1984. 23: p. 568-571.
28. Bircher, N., Safar, P., Open-chest CPR: An old method whose time has returned. Am J Emerg Med, 1984. 2: p. 568-71.
29. McDonald, J., Systolic and mean arterial pressures during manual and mechanical CPR in humans. Ann Emerg Med, 1982. 11: p. 292-5.
30. Ornato, J., et al., Measurement of ventilation during cardiopulmonary resuscitation. Crit Care Med., 1983. 1: p. 79-82.
31. Kim, H., et al., Amelioration of impaired cerebral metabolism after severe acidotic ischemia by tirilazad post-treatment in dogs. . Stroke, 1996. 27: p. 114-21.
32. Iwatsuki, N., et al., Hyperbaric oxygen combined with nicardipine administration accelerates neurologic recovery after cerebral ischemia in a canine model. . Crit Care Med, 1994. 22: p. 858-63.
33. Cervantes, M., Moralı´, G, Letechipı´a-Vallejo, G., Melatonin and ischemia reperfusion injury of the brain. J. Pineal Res, 2008. 45: p. 1-7.
34. Krep, H., Bernd W, Bottiger, BW, et al., Time course of circulatory and metabolic recovery of cat brain after cardiac arrest assessed by perfusion- and diffusion-weighted imaging and MR-spectroscopy. Resuscitation, 2003. 58: p. 337-348.
35. DeGraba, T., Pettigrew, C., Why do neroprotectivedrugs work in animals but not in humans? Neurologic Clinics, 2000. 18: p. 475-493.
36. Ginsberg, M., Adventures in the Pathophysiology of Brain Ischemia: Penumbra, Gene Expression, Neuroprotection. The 2002 Thomas Willis Lecture. Stroke, 2003. 34: p. 214-223.
37. Cheng, J., Al-Khoury, L, Zivin, JA., Neuroprotection for Ischemic Stroke: Two Decades of Success and Failure. NeuroRX, 2004. 1: p. 36-45.
38. Roine, R.O., et al., Nimodipine after resuscitation from out-of-hospital ventricular fibrillation. A placebo-controlled, double-blind, randomized trial. JAMA, 1990. 264(24): p. 3171-3177.
39. Longstreth, W.T., Jr., et al., Randomized clinical trial of magnesium, diazepam, or both after out-of-hospital cardiac arrest. Neurology, 2002. 59(4): p. 506-514.
40. Landau, W.M., et al., Randomized clinical trial of magnesium, diazepam, or both after out-of-hospital cardiac arrest. Neurology, 2003. 60(11): p. 1868-1869.
41. Halstrom, A., Rea, TD, et al., Manual chest compression vs use of an automated chest compression device during resuscitation following out-of-hospital cardiac arrest: a randomized trial. JAMA, 2006. 295: p. 2620-8.
42. Lafuente-Lafuente, C., Melero-Bascones, M., Active chest compression-decompression for cardiopulmonary resuscitation. Cochrane Database Syst Rev., 2004. (2):CD002751.
43. Aung, K., Htay, T., Vasopressin for cardiac arrest: a systematic review and meta-analysis. Arch Intern Med, 2005. 10: p. 17-24.
44. Callaham, M., Madsen, CD, Barton, CW, Saunders, CE, Pointer, J., A randomized clinical trial of high-dose epinephrine and norepinephrine vs standard-dose epinephrine in prehospital cardiac arrest. JAMA, 1992. 268: p. 2667-72.
45. Rincon, F., Mayer, SA., Therapeutic hypothermia for brain injury after cardiac arrest. . Semin Neurol 2006. 26: p. 387-395.
46. Bernard, S., Gray, TW, Buist, MD, et al., Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med, 2002. 346: p. 557-563.
47. Liu, L. and M.A. Yenari, Therapeutic hypothermia: neuroprotective mechanisms. Front Biosci, 2007. 12: p. 816-25.
48. The-Hypothermia-after-Cardiac-Arrest-Study-Group, Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med, 2002. 346: p. 549-556.
49. Nolan, J., Morley, PT, Vanden Hoek, TL, Hickey, RW., Therapeutic Hypothermia After Cardiac Arrest: An Advisory Statement by the Advanced Life Support Task Force of the International Liaison Committee on Resuscitation. Circulation, 2003. 108: p. 118-121.
50. Arrich, J., Clinical application of mild therapeutic hypothermia after cardiac arrest. Crit Care Med, 2007. 35(4): p. 1041-7.
51. Sandroni, C., et al., In-hospital cardiac arrest: incidence, prognosis and possible measures to improve survival. Intensive Care Med, 2007. 33(2): p. 237-45.
52. Safar, P., Resuscitation from clinical death: Pathophysiologic limits and therapeutic potentials. Crit Care Med, 1988. 16: p. 923-941.
53. Safar, P., et al., Improved cerebral resuscitation from cardiac arrest in dogs with mild hypothermia plus blood flow promotion. Stroke, 1996. 27(1): p. 105-13.
54. Polderman, K.H., Hypothermia and neurological outcome after cardiac arrest: state of the art. Eur J Anaesthesiol Suppl, 2008. 42: p. 23-30.
55. Busto, R., Dietrich, WD, Globus, MY, et al., Small differences in intraischemic brain temperature critically determine the extent of ischemic neuronal injury. J Cereb Blood Flow Metab, 1987. 7: p. 729-738.
56. Safar, P., Behringer, W., ed. Brain resuscitation after cardiac arrest. Textbook of neurointensive care., ed. A. Layon, Gabrielli, A, Friedman, WA (Eds). . 2001, WB Saunders: Philadelphia.
57. Shimohata, T., H. Zhao, and G.K. Steinberg, Epsilon PKC may contribute to the protective effect of hypothermia in a rat focal cerebral ischemia model. Stroke, 2007. 38(2): p. 375-80.
58. Zhao, H., G.K. Steinberg, and R.M. Sapolsky, General versus specific actions of mild-moderate hypothermia in attenuating cerebral ischemic damage. J Cereb Blood Flow Metab, 2007. 27(12): p. 1879-94.
59. American-Heart-Association, AHA CPR Guidelines: Part 7.2: Management of Cardiac Arrest. Circulation, 2005. 112:IV-58-IV-66.
60. Abella, B., Rhee, JW, Huang, KN, et al., Induced hypothermia is underused after resuscitation from cardiac arrest: A current practice survey. Resuscitation, 2005. 64: p. 181-186.
61. Merchant, R., Soar, J, Skrifvars, MB, et al., Therapeutic hypothermia utilization among physicians after resuscitation from cardiac arrest. . Crit Care Med, 2006. 34: p. 1935-1940.
62. Kennedy, J., Green, RS, Stenstrom, R., The use of induced hypothermia after cardiac arrest: A survey of Canadian emergency physicians. CJEM, 2008. 10: p. 125-130.
63. Suffoletto, B., Salcido, DD, Menegazzi, JJ., Use of prehospital-induced hypothermia after out-of-hospital cardiac arrest: A Survey of the National Association of Emergency Medical Services Physicians. Prehosp Emerg Care, 2008. 12: p. 52-56.
64. Alam, H., Just do it. Critical care medicine,, 2008. 36: p. 2456-7.
65. Skulec, R., et al., Induction of mild hypothermia in cardiac arrest survivors presenting with cardiogenic shock syndrome. Acta Anaesthesiol Scand, 2008. 52(2): p. 188-94.
66. Hay, A.W., et al., Therapeutic hypothermia in comatose patients after out-of-hospital cardiac arrest. Anaesthesia, 2008. 63(1): p. 15-9.
67. Wolfrum, S., et al., Mild therapeutic hypothermia in patients after out-of-hospital cardiac arrest due to acute ST-segment elevation myocardial infarction undergoing immediate percutaneous coronary intervention. Crit Care Med, 2008. 36(6): p. 1780-6.
68. Bernard, S., Therapeutic hypothermia after cardiac arrest: now a standard of care. Crit Care Med, 2006. 34(3): p. 923-4.
69. Wolff, B., et al., Early achievement of mild therapeutic hypothermia and the neurologic outcome after cardiac arrest. Int J Cardiol, 2008.
70. Nagel, S., et al., Therapeutic hypothermia in experimental models of focal and global cerebral ischemia and intracerebral hemorrhage. Expert Rev Neurother, 2008. 8(8): p. 1255-68.
71. Nozari, A., et al., Critical time window for intra-arrest cooling with cold saline flush in a dog model of cardiopulmonary resuscitation. Circulation, 2006. 113(23): p. 2690-6.
72. Reich, H., et al., Cardiac resuscitability with cardiopulmonary bypass after increasing ventricular fibrillation times in dogs. Ann Emerg Med, 1990. 19(8): p. 887-90.
73. Angelos, M., P. Safar, and H. Reich, A comparison of cardiopulmonary resuscitation with cardiopulmonary bypass after prolonged cardiac arrest in dogs. Reperfusion pressures and neurologic recovery. Resuscitation, 1991. 21(2-3): p. 121-35.
74. Radovsky, A., et al., Regional prevalence and distribution of ischemic neurons in dog brains 96 hours after cardiac arrest of 0 to 20 minutes. Stroke, 1995. 26(11): p. 2127-33; discussion 2133-4.
75. Thoresen, M., Wyatt, J. [see comments], Keeping a cool head, post-hypoxic hypothermia: an old idea revisited. Acta Paediatr 1997. 86: p. 1029-33.
76. Nozari, A., et al., Mild hypothermia during prolonged cardiopulmonary cerebral resuscitation increases conscious survival in dogs. Crit Care Med, 2004. 32(10): p. 2110-6.
77. Kuboyama, K., Safar, P, Radovsky, A, Tisherman, SA, Stezoski, SW, Alexander, H., Delay in cooling negates the beneficial effect of mild resuscitative cerebral hypothermia after cardiac arrest in dogs: a prospective, randomized study [see comments]. 21, 1993. Crit Care Med: p. 1348-58.
78. Takata, K., Takeda, Y, Sato T, Nakatsuka, H, Yokoyama, M, Morita, K., Effects of hypothermia for a short period on histologic outcome and extracellular glutamate concentration during and after cardiac arrest in rats. . Crit Care Med, 2005. 33: p. 1340 -1345.
79. Abella B, Z.D., Alvarado J, Hamann K, Vanden Hoek T, Becker L., Intra-arrest cooling improves outcomes in a murine cardiac arrest model. Circulation, 2004. 109: p. 2786 -2791.
80. Dietrich, W., Busto, R, Alonso, O, et al. 993, Intraischemic but not postischemic brain hypothermia protects chronically following global forebrain ischemia in rats. J Cerebr Blood Flow Metab, 1993. 13: p. 541-549.
81. Maier, C.M., et al., Delayed induction and long-term effects of mild hypothermia in a focal model of transient cerebral ischemia: neurological outcome and infarct size. J Neurosurg, 2001. 94(1): p. 90-6.
82. Marion, D., Leonov Y, Ginsberg, M, Katz, LM, Kochanek, PM, Lechleuthner, A, Nemoto, EM, Obrist, W, Safar, P, Sterz, F, Tisherman, SA, White, RJ, Xiao, F, Zar, H., Resuscitative hypothermia. Crit Care Med, 1996. 24: p. S81-9.
83. Zivin, J., Editorial comment. Stroke, 1999. 30: p. 1899.
84. Wake-County-Government, Wake County Emergency Medical Services. 2008, Wake County Government.
85. Hinchey, P., et al., Out-of-hospital cardiac arrest survival after the sequential implementation of 2005 AHA guidelines for compressions, ventilations, and induced hypothermia., in SAEM Meeting. 2008: Washington, D.C. .
86. Olson, J., Hinchey, P, Myers, B. (2006) Wake County EMS Cools Down: System begins induced hypothermia of ROSC patients. JEMS Volume,
87. Bayegan, K., et al., Rapid non-invasive external cooling to induce mild therapeutic hypothermia in adult human-sized swine. Resuscitation, 2008. 76(2): p. 291-8.
88. Kurz, A., Sessler, DI, Birnbauer, F, Illievich, U, Spiss, C., Thermoregulatory vasoconstriction impairs active core cooling. Anesthesiology 1995. 82: p. 870-6.
89. Stolwijk, J., Hardy, JD., ed. Control of body temperature: Reactions to environmental agents. In Handbook of Physiology., ed. e. Douglas HK. . 1977, American Physiological Society: Bethesda. 45-69.
90. Doufas, A., Consequences of inadvertent perioperative hypothermia. Best Pract Res Clin Anaesthesiol, 2003. 17: p. 535-49.
91. Sheffield, C., Sessler, DI, Hunt, TK. , Mild hypothermia during isoflurane anesthesia decreases resistance to E. coli dermal infection in guinea pigs. Acta Anaesthesiol Scand, 1994. 38: p. 201-5.
92. Lee, S., Battistella, FD, Go, K., Hypothermia induces T-Cell production of immunosuppressive cytokines. J Surg Res, 2001 100(4): p. 150-153.
93. Reed, R., Bracey, AW, Hudson, JD, Miller, TA, Fisher, RP. , Hypothermia and blood coagulation: dissociation between enzyme activity and clotting factor levels. Circ Shock, 1990. 32: p. 141-152.
94. Nirula, R., Gentilello, LM., ed. Detrimental Effects of Hypothermia Therapeutic Hypothermia., ed. S. Tisherman, Sterz, F. 2007, Springer US: New York.
95. Flores-Maldonado, A., Medina-Escobedo, CE, Rios-Rodriguez, HM, Fernandez-Dominguez, R. , Mild perioperative hypothermia and the risk of wound infection. Arch Med Res, 2001. 32: p. 227-231.
96. Kurz, A., Sessler, DI, Lenhardt, R., Perioperative normothermia to reduce the incidence of surgical wound infection and shorten hospitalization. N Engl J Med, 1996. 334: p. 1209-15.
97. Sheffield, C., Sessler, DI, Hopf, HW, Schroeder, M, Moayeri, A, Hunt, TK, West, JM. , Centrally and locally mediated thermoregulatory responses alter subcutaneous oxygen tension. Wouns Rep Reg 1997. 4: p. 339-45.
98. Wenisch, C., Narzt, E, Sessler, DI. Parschalk, B, Lenhardt, R, Kurz, A, Graninger, W., Mild intraoperative hypothermia reduces production of reactive oxygen intermediates by polymorphonuclear leukocytes. Anesth Analg, 1996. 82: p. 810-6.
99. Beilin, B., Shavit, Y, Razumovsky, J, et al. , Effects of mild perioperative hypothermia on cellular immune responses. Anesthesiology, 1998. 89: p. 1133-1140.
100. Jyung, R., Mustoe, TA., Role of cytokines in wound repair. Clinical Application of Cytokines., ed. J. Oppenheim, Rossio, JL, Gearing, AJH, eds. 1993, New York: Oxford University Press.
101. Baigrie, R., Lamont, PM, Kwiatkowski, D, Dallman, MG, Morris, PG., Systemic cytokine response after major surgery. Br J Surg, 1992. 79: p. 757-60.
102. Qwarnstrom, E., Page, RC, Gillis, S, Dower, SK., Binding, internalization and intracellular localization of interleukin-1 beta in human diploid fibroblasts. B Biol Chem, 1988;. 263:: p. 8261-9.
103. Peterson, K., Carson, S, Carney, N., Hypothermia treatment for traumatic brain injury: a systematic review and meta-analysis. J Neurotrauma, 2008. 25(1): p. 62-71.
104. Hammersborga, S., Brekkea, KB, Haugena, OM, et al., Surface cooling versus core cooling: Comparative studies of microvascular fluid- and protein-shifts in a porcine model. Resuscitation, 2008. 79: p. 292-300.
105. Merchant, R., Abella,BS, Peberdy, MA, Soar, J, et al., Therapeutic hypothermia after cardiac arrest: Unintentional overcooling is common using ice packs and conventional cooling blankets. Crit Care Med, 2006. 34[Suppl.]: p. S490-S494.
106. Al-Senani, F., Graffagnino, C, Grotta, JC, et al., A prospective, multicenter pilot study to evaluate the feasibility and safety of using the CoolGard System and Icy catheter following cardiac arrest. . Resuscitation, 2004. 62(2): p. 143-50.
107. Chen, R., Chien, S., Hemodynamic functions and blood viscosity in surface hypothermia. Am J Physiol Lung Cell Mol Physiol, 1978. 235: p. H136-43.
108. Zarins, C., Skinner, DB., Hemodynamics and blood flow distribution following prolonged circulation at 5 degrees C. Am J Physiol., 1975. 229: p. 275-8.
109. Hammersborga, S., Farstad, M, Haugen, O, Kvalheim, VL, Onarheim, H, Husby, P., Time course variations of haemodynamics, plasma volume and microvascular fluid exchange following surface cooling: an experimental approach to accidental hypothermia. Resuscitation, 2005. 65: p. 211-9.
110. Lewis, T., Swelling of the human limbs in response to immersion in cold water. Clin Sci, 1939. 4.
111. Farry, P., Prentice, NG, Hunter, AC, Wakelin, CA., Ice treatment of injured ligament: an experimental model. N Z Med J. , 1980. 91: p. 12-14.
112. Matthew, C., Sils, IV, Bastille, AM., Tissue-specific extravasation of albumin-bound Evans blue in hypothermic and rewarmed rats. Can J Physiol Pharmacol, 2002. 80(3): p. 233-243.
113. Kruuv, J., Glofcheski, D, Cheng, KH, Campbell, SD, Al-Qysi, HMA, Nolan, WT, Lepock, JR, Factors influencing survival and growth of mammalian cells exposed to hypothermia. I. Effects of temperature and membrane lipid perturbers. J Cell Physiol, 1983. 115: p. 179-185.
114. Rule, G., Frim, J, Thompson, JE, Lepock, JR, Kruuv, J. , Theeffect of membrane lipid perturbers on survival of mammalian cells to cold. Cryobiology 1978. 15: p. 408-414.
115. Marsh, D., Lindell, SL, Fox, LE, Belzer, FO, Southard, JH. , Hypothermic preservation of hepatocytes. I. Role of cell swelling. Cryobiology, 1989. 26: p. 524-534.
116. McAnulty, J., Ametani, MS, Southard, JH, Belzer, FO., Effect of hypothermia on intracellular Ca21 in rabbit renal tubules suspended in UW-gluconate preservation solution. . Cryobiology, 1996. 33: p. 196-204.
117. Breton, S., Brown, D., Cold-induced microtubule disruption and relocalization of membrane proteins in kidney epithelial cells. J Am Soc Nephrol, 1998. 9: p. 155-166.
118. Stefanovich, P.E., RM, Sheehan, SJ, Tompkins, RG, Yarmush, ML., Effects of hypothermia on the function, membrane integrity, and cytoskeletal structure of hepatocytes. Cryobiology, 1995. 23: p. 389-403.
119. Zieger, M., Glofcheski, DJ, Lepock, JR, Kruuv, J. , Factors influencing survival of mammalian cells exposed to hypothermia IV. Effects of iron chelation. . Cryobiology, 1990. 27: p. 452-464.
120. Rauen, R., DeGroot, H., Cold induced release of reactive oxygen species asa decisive mediator of hypotherrmiainjury to cultured liver cells. Free Rad Biol & Med, 1998. 24(7/8): p. 1316-1323.
121. Hochachka, P., Defense strategies against hypoxia and hypothermia. Science 1986. 231: p. 234-241.
122. Endrich, B., Hammersen F, Messmer, K., Microvascular ultrastructure in non-freezing cold injury. Res Exp Med, 1990. 190: p. 365-79.
123. Verrey, F., Groscurth, P, Bolliger, UI., Cytoskeletal disruption in A6 kidney cells: Impact on endo-exocytosis and NaCI transport regulation by antidiuretic hormone. J Membr Bio, 1995. 145: p. 193-204.
124. Hall, S., Komai, H, Reader, J, Haworth, SG. , Donor lung preservation: Effect of cold preservation fluids on cultured pulmonary endothelial cells. . Am J Physiol Lung Cell Mol Physiol, 1994. 267: p. L508-L5 I 7.
125. Breton, S., Brown, D., Cold-induced microtubule disruption and relocalization of membrane proteins inkidney epithelial cells. J Am Soc Nephrol, 1998. 9: p. 155-66.
126. Reed, C., Clark, D, editors, ed. Heat exchangers and hypothermia. Cardiopulmonary Perfusion. 1975, Texas Medical Press, Inc.: Houston TX. 272–8.
127. Furuse, M., Ohta, T, Ikenaga, T, et al., Effects of intravascular perfusion of cooled crystalloid solution on cold-induced brain injury using an extracorporeal cooling-filtration system. Acta Neurochir, 2003. 145: p. 983-993.
128. Behringer, W., et al., Veno-venous extracorporeal blood shunt cooling to induce mild hypothermia in dog experiments and review of cooling methods. Resuscitation, 2002. 54(1): p. 89-98.
129. Overlie, P., Emergency Use of Cardiopulmonary Bypass. Journal of Interventional Cardiology, 1995. 8: p. 239-247.
130. Kurusz, M., Zwischenberger, JB., Percutaneous cardiopulmonary bypass for cardiac emergencies. Perfusion, 2002. 17: p. 269-77.
131. Holzer, M., Behringer, W, Janata, A, Bayegan, K, Schima, H, Deckert, Z, Losert, U, Laggner, AN, Sterz, F., Extracorporeal venovenous cooling for induction of mild hypothermia in human-sized swine. Crit Care Med, 2005. 33: p. 1346-50.
132. Bernard, S., Buist, M, Monterio, O, Smith, K., Induced hypothermia using large volume, ice-cold intravenous fluid in comatose survivors of out-of-hospital cardiac arrest: a preliminary report. Resuscitation, 2003. 56: p. 9-13
133. Bernard, S., Rosalion, A., Therapeutic hypothermia induced during cardiopulmonary resuscitation using large-volume, ice-cold intravenous fluid. Resuscitation, 2008. 76: p. 311 – 313.
134. Kamarainen, A., et al., Prehospital induction of therapeutic hypothermia during CPR: a pilot study. Resuscitation, 2008. 76(3): p. 360-3.
135. Haslam, D., James, WP. , Obesity. Lancet, 2005. 366: p. 1197-209.
136. Feldschuh, J., Enson, Y., Prediction of the normal blood volume. Relation of blood volume to body habitus. Circulation, 1977. 56: p. 605 – 612.
137. Plaisier, B.R., Thoracic lavage in accidental hypothermia with cardiac arrest–report of a case and review of the literature. Resuscitation, 2005. 66(1): p. 99-104.
138. Xiao, F., P. Safar, and H. Alexander, Peritoneal cooling for mild cerebral hypothermia after cardiac arrest in dogs. Resuscitation, 1995. 30(1): p. 51-9.
139. Darwin, M., Leaf, JD, Hixon, HL. Neuropreservation of Alcor patient A-1068. Cryonics 1986 [cited 7 2]; 17-32]. Available from: http://www.alcor.org/Library/html/casereport8504.html.
140. Darwin, M. Cryopreservation Patient Case Report: Arlene Francis Fried, A-1049. 2006 [cited 2007 07 June]; Available from: http://www.alcor.org/Library/html/fried.html.
141. Jones, T., Cryopreservation case report: the cryopreservation of patient A-2063. Cryonics, 2005. 26(1): p. 10-12.
142. Bellamy, R., The causes of death in conventional land warfare: Implications for combat casualty research. Military Medicine, 1984. 149: p. 55-62.
143. Bellamy, R., Death on the battlefield and the role of first aid. Military Medicine, 1987a. 152: p. 634-35.
144. Bellamy, R., Death on the battlefield and the role of first aid. Military Medicine. 1987b. 152 p. 617-21.
145. Bellamy, R., Trauma epidemiology of combat casualties. , in Presentation to Institute of Medicine Committee on Fluid Resuscitation for Combat Casualties. 1998: Washington, D.C.
146. Bowen, T., Bellamy, RF, (eds). , Emergency war Surgery: Second United States Revision of the Emergency War Surgery Handbook. 1998, US Government printing Office: Washington, D.C.
147. Wu, X., et al., Emergency preservation and resuscitation with profound hypothermia, oxygen, and glucose allows reliable neurological recovery after 3 h of cardiac arrest from rapid exsanguination in dogs. J Cereb Blood Flow Metab, 2008. 28(2): p. 302-11.
148. Tisherman, S., Rodriguez, A, Safar, P., Therapeutic hypothermia in traumatology. Surg Clin North Am, 1999. 79: p. 1269-89.
149. www.engineeringtoolbox.com, Dry air properties at temperatures ranging 175 – 1900 K – specific heat capacity, ratio of specific heats, dynamic viscosity, thermal conductivity, Prandtl number, density and kinematic viscosity. 2008.
150. www.engineeringtoolbox.com., Thermal properties of water – density, freezing temperature, boiling temperature, latent heat of melting, latent heat of evaporation, critical temperature and more. 2008.
151. Zikria, B., Ferrer, JM, Malm, JR., Pulmonary hypothermia in dogs. J Appl Physiol 1968. 24: p. 707-10.
152. Harrison, M., Hysing, ES, Bo, G., Control of body temperature: use of respiratory tract as a heat exchanger. J Pediatr Surg, 1977. 12: p. 821-8.
153. Powell, F., Hopkins, SR., Comparative physiology of lung complexity: implications for gas exchange. News in Physiological Science, 2004. 19: p. 55-60.
154. Webb, P., ed. Cold exposure. In: The physiology and medicine of diving., ed. P. Bennett, Elliot, DM, eds. . 1975, Bellaire Tindall: London.
155. Shaffer, T., et al., The effects of liquid ventilation on cardiopulmonary function in preterm and neonatal lambs. Pediatr Res, 1983. 4: p. 303-6.
156. Klystra, J., Survival in air after breathing fluid. Lancet, 1962. 2: p. 1170.
157. Klystra, J., et al., Hydraulic Compression of Mice to 166 Atmospheres. Science, 1967. 158: p. 793-94.
158. Klystra, J., Lanphier, EH., Gas Exchange in Fluid Ventilated Dogs. Fed.Proc, 1964. 23: p. 469.
159. Darwin, M., Liquid ventilation: A bypass on the way to bypass. CryoCare Report, 1996(#7): p. 11-16.
160. Safar, P., Stezoski, W, Nemoto, EM, Safar, P (P.I.). Amelioration of brain damage after 12 minutes’ cardiac arrest in dogs. Brain Resuscitation Clinical Trial I Study Group. Arch Neurol, 1976. 33/2: p. 91-95.
161. Darwin, M., Russell, S, Rasch, C, O’Farrell, J, Harris, S., A novel method of rapidly inducing or treating hypothermia or hyperpyrexia, by means of ‘mixed-mode’ (gas and liquid) ventilation using perfluorochemicals., in In: Society of Critical Care Medicine 28th Educational and Scientific Symposium. 1999, Critical Care Medicine: San Francisco. p. A81.
162. Taylor, R., et al., Design of the mammalian respiratory system. III. Scaling maximum aerobic capacity to body mass: Wild and domestic mammals. Respir Physiol, 1981. 44: p. 25-37.
163. Clark, L., Gollin, F., Survival of Mammal Breathing Organic Liquid Equilibrated with Oxygen at Atmospheric Pressure. Science, 1966: p. 1755.
164. Leach, C., et al., Perfluorocarbon associated gas exchange (partial liquid ventilation) in respiratory syndrome: A prospective, randomized, controlled study. Crit Care Med, 1993. 21: p. 1270-8.
165. Hirschl, R., Pranikoff, T, Gauger, P, et al., Liquid ventilation in adults, children and neonates. Lancet, 1995. 346: p. 1201-2.
166. Varani, J.H., RB, Dame, M, Johnson, K., Perfluorocarbon protects lung epithelial cells from neutrophil-mediated injury in an in vitro model of liquid ventilation therapy. Shock, 1996. 6(5): p. 339-44.
167. Hirschl, R., Tooley, R, Parent, AC, Johnson, K, Bartlett, RH., Improvement of gas exchange, pulmonary function, and lung injury with partial liquid ventilation. A study model in a setting of severe respiratory failure. Chest, 1995. 108(2): p. 500-8.
168. Uihlein, A., Theye, RA, Dawson, B, et al., The use of profound hypothermia, extracorporeal circulation and total circulatory arrest for an intracranial aneurysm. Preliminary report with reports of cases. Mayo Clin Proc, 1960. 35: p. 567-576.
169. Michenfelder, J.D., et al., Profound Hypothermia and Total Circulatory Arrest in Neurosurgery: Methods, Results and Physiologic Effects. Acta Neurochir Suppl, 1964. 20: p. SUPPL 13:159+.
170. Woodhall, B., Sealy, WC, Hall, KD, et al., Craniotomy under conditions of quinidine-protected cardioplegia and profound hypothermia. Ann Surg, 1960. 152: p. 37-44.
171. Du Bouchet, N., E. Prochiant, and B. Latscha, [Cardiac arrest induced by deep hypothermia. Its superiority over other technics.]. Anesth Analg (Paris), 1962. 19: p. 239-50.
172. Vigouroux, R., et al., [Hypothermia and cardiac arrest. (Considerations on a case of recuperation after 80 minutes of ventricular fibrillation)]. Mars Chir, 1962. 14: p. 102-6.
173. Benson, D.W., et al., The use of hypothermia after cardiac arrest. Anesth Analg, 1959. 38: p. 423-8.
174. Feldman, E., B. Rubin, and S.N. Surks, Beneficial effects of hypothermia after cardiac arrest. J Am Med Assoc, 1960. 173: p. 499-501.
175. Lore, J.M., S.G. Gordon, and E.W. Gordon, Successful use of hypothermia following cardiac arrest in twelve-day-old infant. N Y State J Med, 1960. 60: p. 278-9.
176. Gravel, J.A., J.P. Dechene, and M. Beaulieu, [Hypothermia in the prevention of cerebral lesions following cardiac arrest.]. Laval Med, 1960. 29: p. 48-60.
177. Barone, F., Feuerstein, GZ, White, RF., Brain cooling during transient focal ischemia provides complete neuroprotection. Neurosci Biobehav Rev, 1997. 21: p. 31-44.
178. Bell, T.E., G.L. Kongable, and G.K. Steinberg, Mild hypothermia: an alternative to deep hypothermia for achieving neuroprotection. J Cardiovasc Nurs, 1998. 13(1): p. 34-44.
179. Yenari, M.A. and H.S. Han, Influence of hypothermia on post-ischemic inflammation: role of nuclear factor kappa B (NFkappaB). Neurochem Int, 2006. 49(2): p. 164-9.
180. Krieger, D.W. and M.A. Yenari, Therapeutic hypothermia for acute ischemic stroke: what do laboratory studies teach us? Stroke, 2004. 35(6): p. 1482-9.
181. Corbett, D., Thornhill, J. , Temperature modulation (hypothermic and hyperthermic conditions) and its influence on histological and behavioral outcomes following cerebral ischemia. Brain Pathol, 2000. 10: p. 145-52.
182. Reed, C., Clark, D. , Heat exchangers and hypothermia. Cardiopulmonary Perfusion. 1975: Texas Medical Press, Inc. 272-8.
183. Darwin, M., Cryopreservation of CryoCare Patient C-2150. CryoCare Report #6, January, 1999: p. 4-16.
184. Notebook MPI: 3M Performance Fluids. 1995, St Paul MN: 3M Company.
185. Giesbrecht, G., Bristow, GK., A second postcooling afterdrop: more evidence for a convective mechanism. J Appl Physiol, 1992. 73: p. 1253-8.
186. Clark, L., Jr, Hoffmann, RE, Davis, SL., Response of the rabbit lung as a criterion of safety for fluorocarbon breathing and blood substitutes. . Biomater Artif Cells Immobilization Biotechnol, 1992. 20: p. 1085-99.
187. Yannopoulos, D., Nadkarni, VM, McKnite, SH, Rao, A, Kruger, K, Metzger, J, Benditt, D, Lurie,KJ., Intrathoracic pressure regulator during continuous-chest-compression advanced cardiac resuscitation improves vital organ perfusion pressures in a porcine model of cardiac arrest. Circulation, 2005. 112: p. 803-81.
188. Lurie, K.Z., T, McKnite, S., The use of an inspiratory impedance valve improves neurologically intact survival in a porcine model of ventricular fibrillation. Circulation, 2002. 105: p. 124 -129.
189. Lurie, K., Zielinski, T, Voelckel, W, et al., Augmentation of ventricular preload during treatment of cardiovascular collapse and cardiac arrest. Crit Care Med 2002. 30: p. (Suppl):S162-5.
190. Miyamoto, Y., Mikami, T., Maximum capacity of ventilation and efficiency of gas exchange during liquid breathing in guinea pigs. Jpn J Physiol 1976. 26: p. 603-18.
191. Koen, P., Wolfson, MR, Shaffer, TH., Fluorocarbon ventilation: maximal expiratory flows and CO2 elimination. Pediatr Res, 1988. 24: p. 291-6.
192. Matthews, W., Balzer, RH, Shelburne, JD, Pratt, PC, Kylstra, JA., Steady-state gas exchange in normothermic, anesthetized, liquid ventilated dogs. Undersea Biomed Res, 1978. 5: p. 341-54.
193. Reece, W., ed. Respiration in mammals. In Duke’s Physiology of Domestic Animals, 10th Edition, ed. e. Swenson M. 1987, Comstock Publishing Associates: London. 235–7.
194. Yu, C., Jimenez, O, Marcillo, AE, Weider, B, Bangerter, K, Dietrich, WD, Castro, S, Yezierski, RP., Beneficial effects of modest systemic hypothermia on locomotor function and histopathological damage following contusion-induced spinal cord injury in rats. J Neurosurg, 2000. 93(1 Suppl): p. 85-93.
195. Ha, K., Kim, YH., Neuroprotective effect of moderate epidural hypothermia after spinal cord injury in rats. Spine, 2008. 33: p. 2059-65.
196. Shibuya, S., Miyamoto, O, Janjua, NA, Itano, T, Mori, S, Norimatsu, H., Post-traumatic moderate systemic hypothermia reduces TUNEL positive cells following spinal cord injury in rat. Spinal Cord, 2004. 42: p. 29-34.
197. Safar, P., Cerebral resuscitation (Letter). Ann Emerg Med, 1993;. 22: p. 759.
198. Safar, P., On the Future of Reanimatology. Academic Emergency Medicine, 2000. 7(1): p. 75-89.
199. Schmid-Elsaesser, R., Hungerhuber, E, Zausinger, S, Baethmann, A, Reulen, HJ., Combination drug therapy and mild hypothermia: a promising treatment strategy for reversible, focal cerebral ischemia. Stroke, 1999. 30: p. 1891-9.
200. Rose, G., Cold weather and ischaemic heart disease. Br J Prev Soc Med 1966. 20: p. 97-100.
201. Anderson, T., Rochard, C., Cold snaps, snowfall and sudden death from ischaemic heart disease. Can Med Assoc, 1979. 121: p. 1580-3.
202. Epstein, S., Stampfer, M, Beiser, GD, Goldstein, RE, Braunwald, E., Effects of a reduction in environmental temperature on the circulatory response to exercise in man. Implications concerning angina pectoris. N Engl J Med, 1969. 280: p. 7-11.
203. Hayward, J., Holmes, WF, Gooden, BA., Cardiovascular responses in man to a stream of cold air. Cardiovasc Res 1976. 10: p. 691-6.
204. Velasco, M., Gómez, J, Blanco, M, Rodriguez, I., The cold pressor test: pharmacological and therapeutic aspects. Am J Ther, 1997. 4: p. 34-8.
205. Gondi, B., Nanda, NC., Evaluation of coronary artery disease by cold pressor two-dimensional echocardiography. Circulation, 1981. 64: p. Abstracts of 54th scientific sessions of American Heart Association, iv-14.
206. Mudge, G., Grossman,W, Mills, RM, Lesch, M, Braunwald, E., Reflex increase in coronary vascular resistance in patients with ischaemic heart disease. . N Engl J Med, 1976. 295(1): p. 333-7.
207. Raizner, A., Chahine, RA, Ishimori, T, Verani, MS, Zacca, N, Jamal, N, Miller, RR, Luchi, RJ., Provocation of coronary artery spasm by the cold pressor test. Hemodynamic, arteriographic and quantitative angiographic observations. Circulation, 1980. 62: p. 925-932.
208. Hattenhauer, M., Neil, WA., The effect of cold air inhalation on angina pectoris and myocardial oxygen supply. Circulation, 1975. 51: p. 1053-8.
209. Lassvik, C., Areskog, NH., Angina pectoris during inhalation of cold air reactions to exercise. Br Heart J, 1980. 43: p. 661-7.
210. Dodds, P., Bellamy, CM, Muirhead, RA, Perry, RA., Vasoconstrictor peptides and cold intolerance in patients with stable angina pectoris. Heart, 1995. 73: p. 25-31.
211. Maggiore, Q., Pizzarelli, F, Sisca, S, et al., Blood temperature and vascular stability during hemodialysis and hemofiltration. Trans Am Soc Artif Intern Organs, 1982. 28: p. 523-527.
212. Pizzarelli, F., Sisca, S, Zoccali, C, et al., Blood temperature and vascular stability in hemofiltration. Int J Artif Organs, 1983. 6: p. 37-41.
213. Sherman, R., Faustino, EF, Bernholc, AS, Eisinger, RP., Effect of variations in dialysate temperature on blood pressure during hemodialysis. Am J Kidney Dis, 1984. 4: p. 66-68.
214. Kishimoto, T., Yamamoto, T, Shimuzu, G, et al., Cardiovascular stability in low temperature dialysis. Dial Transplant, 1986. 15: p. 329-333.
215. Selby, N., McIntyre, CW., A systematic review of the clinical effects of reducing dialysate fluid temperature. Nephrol Dial Transplant, 2006. 21: p. 1883-1898.
216. Mahida, B., Duler, F, Zasuwa, G, Fleig, G, Levin, NW., Effect of cooled dialysate on serum catecholamines and blood pressure stability. Trans Am Soc Artif Intern Organs, 1983. 29: p. 384-389.
217. Pizzarelli, F., Fom cold to isothermic dialysis: a twenty-five year voyage. Nephrol Dial Transplant, 2007. 22: p. 1007-1012.
218. Maggiore, Q., Enia, G, Catalano, C, Misefari, V, Mundo, A., Effect of blood cooling on cuprophan-induced anaphylotoxin generation. Kidney Int, 1987. 32: p. 908-911.
219. Raja, R., Kramer, M, Alvis, R, Goldstein, S, DeLosAngeles, A., Effect of varying dialysate temperature on hemodialysis hypoxemia. Trans Am Soc Artif Organs, 1984. 30: p. 15-17.
220. Behringer, W., Kittler, H., Sterz, F, Domanovits, H, Schoerkhuber, W, Holzer, M, Mullner, M, Laggner, AN., Cumulative epinephrine dose during cardiopulmonary resuscitation and neurologic outcome. Annals of Internal Medicine, 1998. 129: p. 450-456.
221. Adgey, A., Johnston PW., Approaches to modern management of cardiac arrest. Heart, 1998. 80: p. 397-401.
222. Rhee, B., Zahng, Y Boddicker, KA, Davies, LR, Kerber, RE., Effect of hypothermia on transthoracic defibrillation in a swine model . Resuscitation, 2005. 65: p. 79-85.
223. Wira, C., et al., Resuscitation, 2006. 69: p. 509-16.
224. Boddicker, K., Zang, Y, Zimmerman, B, Davies, LR, Kerber, RE., Hypothermia Improves Defibrillation Success and Resuscitation Outcomes From Ventricular Fibrillation. Circulation, 2005. 111: p. 3195-3201.
225. Martin, D., Garcia, J, Valer, CR, Khuri, SF. , The effects of normothermic and hypothermic cardiopulmonary bypass on defibrillation energy requirements and transmyocardial impedance. Implications for implantable cardioverter-defibrillator implantation. The Journal of Thoracic and Cardiovascular Surgery, 1995. 109(5): p. 981-988.
226. Ujhelyi, M., Sims, JJ, Dubin, SA, Vender, JM, Miller, WA., Defibrillation energy requirements and electrical heterogeneity during total body hypothermia. Crit Care Med, 2001. 29(5): p. 1006-1011.
227. Rankin, A., Rae, AP., Cardiac arrhythmias during rewarming of patients with accidental hypothermia. Br Med J 1984. 289: p. 874-7.
228. Covino, B., Charleston, DA, D’Amato, HE., Ventricular fibrillation in the hypothermic dog. . Am J Physiol Lung Cell Mol Physiol, 1954. 178: p. 148-54.
229. Okada, M., The cardiac rhythm in accidental hypothermia. J Electrocardiol, 1984. 17: p. 123-8.
230. Alexander, L., The treatment of shock from prolonged exposure to cold, especially in water., S.R.A. C.I.O.S. Target Medical Combined Intelligence Objectives Subcommittee. G-S Division, Editor. 1945, Office of the Publication Board, Department of Commerce, Washington D.C.
231. Reuler, J., Hypothermia: Pathophysiology, clinical setting, and management. Ann Intern Med, 1978. 89: p. 519-527.
232. Southwick, F., Dalglish, PH, Jr., Recovery after prolonged asystolic cardiac arrest in profound hypothermia: a case report and literature review. JAMA, 1980. 243: p. 1250-3.
233. Mortensen, E., Berntsen, R, Tveita, T, Lathrop, DA, Refsum, H., Changes in ventricular fibrillation threshold during acute hypothermia. A model for future studies. J Basic Clin Physiol Pharmacol, 1993. 4: p. 313-9.
234. Baumgardner, J., Baranov, D, Smith, DS, Zager, EL., The effectiveness of rapidly infused Intravenous fluids for inducing moderate hypothermia in neurosurgical patients. Anesth Analg, 1999. 89: p. 163-9.
235. Rajek, A., Greif ,R ,Sessler, DI, Baumgardner, J, Laciny, S, Bastanmehr, H., Core Cooling by Central Venous Infusion of Ice-cold (4°C and 20°C) Fluid. Anesthesiology, 2000. 93.
236. Virkkunen, I., Yli-Hankala, A, Silfvast, T., Induction of therapeutic hypothermia after cardiac arrest in prehospital patients using ice-cold Ringer’s solution: a pilot study. Resuscitation, 2004. 62: p. 299-302.
237. Baba, A., Kim, YK, Zhang, H, Liu, M, Slutsky, AS., Perfluorocarbon blocks tumor necrosis factor-alpha-induced interleukin-8 release from alveolar epithelial cells in vitro. Crit Care Med, 2000. 28: p. 1113-18.
238. Kliegel, A., Janata, A, Wandaller, C, et al., Cold infusions alone are effective for induction of therapeutic hypothermia but do not keep patients cool after cardiac arrest. Resuscitation, 2007. 73 p. 46-53.
239. Nordmark, J., Rubertsson, M., Induction of mild hypothermia with infusion of cold (4 ◦C) fluid during ongoing experimental CPR. Resuscitation, 2005. 66: p. 357-365.
240. Cohen, T., Tucker, KJ, Redberg, RF, Lurie, KG, Chin, MC, Dutton, JP, Scheinman, MM., Active compression-decompression resuscitation: a novel method of cardiopulmonary resuscitation. Am Heart J, 1992. 124: p. 1145-50.
241. Cabrini, L., Beccaria, P, Landoni, G, Biondi-Zoccai, GG, Sheiban, I, Cristofolini, M, Fochi, O, Maj, G, Zangrillo, A., Impact of impedance threshold devices on cardiopulmonary resuscitation: a systematic review and meta-analysis of randomized controlled studies. Crit Care Med, 2008. 36: p. 1625-32.
242. Lurie, K., Voelckel, W, Plaisance, P, et al., Use of an inspiratory impedance threshold valve during cardiopulmonary resuscitation: A progress report. Resuscitation, 2000. 44: p. 219-30.
243. Plaisance, P., Lurie, K, Payen, D., Inspiratory impedance during active compression decompression cardiopulmonary resuscitation: a randomized evaluation in patients in cardiac arrest. . Circulation, 2000. 10: p. 989-994.
244. Wolcke, B., Mauer, DK, Schoefmann, MF, Teichmann, H, Provo, TA, Lindner. KH, Dick WF, Aeppli D, Lurie KG., Comparison of standard cardiopulmonary resuscitation versus the combination of active compression-decompression cardiopulmonary resuscitation and an inspiratory threshold device for out-of-hospital cardiac arrest. Circulation, 2003. 108: p. 2201-2205.
245. Jellinek, H., Krenn, H, Oczenski, W, et al., Influence of positive airway pressure on the pressure gradient for venous return in humans. J Appl Physiol, 2000. 88: p. 926-932.
246. Aufderheide, T., Lurie, KG., Death by hyperventilation: A common and life-threatening problem during cardiopulmonary resuscitation. Crit Care Med, 2004. 32(No. 9 (Suppl.)): p. S345–S351.
247. Aufderheide, T., Sigurdsson, G, Pirrallo, RG, et al. , Hyperventilation-induced hypotension during cardiopulmonary resuscitation. Circulation, 2004. 109: p. 1960-1965.
248. Cheifetz, I., Craig, DM, Quick, G, et al., Increasing tidal volumes and pulmonary overdistention adversely affect pulmonary vascular mechanics and cardiac output in a pediatric swine model. Crit Care Med, 1998. 26: p. 710-716.
249. Fewell JE, A.D., Carlson CJ, et al., Continuous positive-pressure ventilation decreases right and left ventricular end diastolic volumes in the dog. Circ Res, 1980. 46: p. 125-132.
250. O’Neil, J., Deakin, CD., Do we hyperventilate cardiac arrest patients? Resuscitation, 2007. 73: p. 82-85.
251. Guerci, A., Shi, AY, Levin, H, Tsitlik, J, Weisfeldt, ML, Chandra, N., Transmission of Intrathoracic Pressure to the Intracranial Space during Cardiopulmonary Resuscitation in Dogs. Circ Res, 1985. 56: p. 20-30.
252. Srinivasana, V., Nadkarnia, VA, Yannopoulosb, D, Marinoa, BS, Sigurdssonc, G, McKnitec, SH, Zookc, M, Bendittc, DG, Lurie, KG., Spontaneous gasping decreases intracranial pressure and improves cerebral perfusion in a pig model of ventricular fibrillation. Resuscitation, 2006. 69: p. 329-334.
253. Chandra, N.C., et al., Observations of hemodynamics during human cardiopulmonary resuscitation. Crit Care Med, 1990. 18: p. 929-34.
254. Weil, M., Rackow, EC, Trevino, R, Grundler, W, Falk, JL, Griffel, MI., Difference in acid-base state between venous and arterial blood during cardiopulmonary resuscitation. N Engl J Med, 1986. 315: p. 153-156.
255. Sigurdsson, G., Yannopoulos, D, McKnite, S, et al., Lowering of intrathoracic pressure improves blood pressure and survival rates in a porcine model of hemorrhagic shock. Resuscitation, 2006. 68: p. 399-404.
256. Rudikoff, M., Maughan, WL, Effron, M. Freund. P, Weisfeldt, ML., Mechanisms of blood flow during cardiopulmonary resuscitation. Circulation, 1980. 61: p. 345-352.
257. Maier, G., Tyson, GS. Olsen, CO, Kerstein, KH, Davis, JW, Conn, A,. Sabiston, DW, Jr., Rankin, JS., The physiology of external cardiac massage: high-impulse cardiopulmonary resuscitation. Circulation 1984. 70: p. 86-101.
258. Frenneaux, A., Haemodynamics of cardiac arrest and resuscitation. Curr Opin Crit Care, 2006. 12: p. 198-203.
259. Kouwenhoven, W., Jude, JR, Knickerbocker, GG., Closed-chest cardiac massage. JAMA 1960. 173: p. 1064-1067.
260. Redberg, R., Tucker, KJ, Cohen, TJ, Dutton, JP, Callaham, ML, Schiller, NB., Physiology of blood flow during cardiopulmonary resuscitation. A transesophageal echocardiographic study. Circulation 1993. 88: p. 534-542.
261. Weisfeldt, M., Chandra, N., Physiology of cardiopulmonary resuscitation. Ann Rev Med, 1981. 32: p. 43-42.
262. Niemann, J., Garner, D, Rosborough, J, Criley, JM., The mechanism of blood flow in closed chest cardiopulmonary resuscitation. Circulation, 1979. 59 & 60: p. I1-74.
263. Niemann, J.R., JP, Hausknecht, M, Garner, D, Criley, JM., Pressure-synchronised cineangiography during experimental cardiopulmonary resuscitation. Circulation, 1981: p. 985-991.
264. Haas, T., Voelcke,l WG; Wenzel, V,Antretter, H, Dessl, A, Lindner, K.H., Revisiting the cardiac versus thoracic pump mechanism during cardiopulmonary resuscitation. Resuscitation 2003. 58: p. 113-116.
265. Werner, J., Greenem, HL, Janko, CK, Cobb, LA., Visualization of cardiac valve motion in man during external chest compression using two-dimensional echocardiography. Implications regarding the mechanism of blood flow. Circulation, 1981. 63: p. 1417-1421.
266. Cohen, J., Chandra, N, Alderson,PO, van Aswegen, A, Tsitlik, JE, Weisfeldt, ML., Timing of pulmonary and systemic blood flow during intermittent high intrathoracic pressure cardiopulmonary resuscitation in the dog. . Am J Cardiol, 1982. 49: p. 1883-1889.
267. Rich, S., Wix, HL, Shapiro, EH., Clinical assessment of heart chamber size and valve motion during cardiopulmonary resuscitation by two-dimensional echocardiography. Am Heart J 1981. 102: p. 368-373.
268. Feneley, M., Maier, GW, Gaynor, JW, Gall, SA, Kisslo, JA, Davis, JW, Rankin, JS., Sequence of mitral valve motion and transmitral blood flow during manual cardiopulmonary resuscitation in dogs. Circulation, 1987. 76: p. 363-375.
269. Deshmukh, H., Weil, MH, Rackow, EW, Trevino, R, Bisera, J., Echocardiographic observations during cardiopulmonary resuscitation: A preliminary report. J.Crit Care Med, 1985. 13: p. 904-906.
270. Ma, M., Hwang, JJ, Lai, LP, et al., Transesophageal echocardiographic assessment of mitral valve position and pulmonary venous flow during cardiopulmonary resuscitation in humans. . Circulation 1995. 92: p. 854-861.
271. Hong, S.B., et al., Physiologic characteristics of cold perfluorocarbon-induced hypothermia during partial liquid ventilation in normal rabbits. Anesth Analg, 2002. 94(1): p. 157-62, table of contents.
272. Harris, S., et al., Rapid (0.5°C/min) minimally invasive induction of hypothermia using cold perfluorochemical lung lavage in dogs. Resuscitation, 2001. 50: p. 189-204.
273. Ko, A.C., et al., Segmental hemodynamics during partial liquid ventilation in isolated rat lungs. Resuscitation, 2003. 57(1): p. 85-91.
274. Beznak, M., Cardiac output during the development of cardiac hypertrophy in the rat. Circ Res, 1958. 6: p. 207-212.
275. Tissier, R., et al., Total liquid ventilation provides ultra-fast cardioprotective cooling. J Am Coll Cardiol, 2007. 49(5): p. 601-5.
276. Schwartz, L., Verbinski, SG, Vander Heide, RS, Reimer, KA., Epicardial temperature is a major predictor of myocardial infarct size in dogs. J Mol Cell Cardiol, 1997. 29: p. 1577- 83.
277. Dixon, S., Whitbourn, RJ, Dae, MW, et al., Induction of mild systemic hypothermia with endovascular cooling during primary percutaneous coronary intervention for acute myocardial infarction. J Am Coll Cardiol 2002. 40: p. 1928 -34.
278. Miki, T., Liu GS, Cohen, MV, Downey, JM., Mild hypothermia reduces infarct size in the beating rabbit heart: a practical intervention for acute myocardial infarction? Basic Res Cardiol, 1998. 93: p. 372- 83.
279. Hale, S., Dave, RH, Kloner, RA., Regional hypothermia reduces myocardial necrosis even when instituted after the onset of ischemia. Basic Res Cardiol, 1997. 92: p. 351-7.
280. Hale, S., Kloner, RA., Myocardial temperature reduction attenuates necrosis after prolonged ischemia in rabbits. Cardiovasc Res 1998;. 40: p. 502-7.
281. Hale, S., Dae, MW, Kloner, RA., Hypothermia during reperfusion limits ‘no-reflow’ injury in a rabbit model of acute myocardial infarction. Cardiovasc Res, 2003. 59: p. 715-22.
282. Koreny, M., et al., Effect of cooling after human cardiac arrest on myocardial infarct size. Resuscitation, 2008.
283. Magid, D., Wang, Y, Herrin J, et al., Relationship between time of day, day of week, timeliness of reperfusion, and in-hospital mortality for patients with acute ST-segment elevation myocardial infarction. JAMA, 2005. 294: p. 803-12.
284. Staffey, K.S., et al., Liquid ventilation with perfluorocarbons facilitates resumption of spontaneous circulation in a swine cardiac arrest model. Resuscitation, 2008. 78(1): p. 77-84.
285. Gentilello, L., Cortes, V, Moujaes, S, Viamonte, M, Malinin, TL, Ho, C, Gomez, GA., Continuous arteriovenous rewarming: experimental results and thermodynamic model simulation of treatment for hypothermia. J Trauma, 1990. 30: p. 1436-49.
286. Hoedemaekers, C., Ezzahti, M, Gerritsen, A, van der Hoeven, JG., Comparison of cooling methods to induce and maintain normo- and hypothermia in intensive care unit patients: a prospective intervention study. Critical Care, 2007. 11: p. R91.
287. Cox, C., Wolfson, MR, Shaffer, TH., Liquid ventilation: a comprehensive overview. Neonatal Netw 1996. 15: p. 31-43.
288. Shiozaki, T., Hayakata, T, Taneda, M, Nakajima, Y, Hashiguchi, N, Fujimi, S, Nakamori, Y, Tanaka, H, Shimazu, T, Sugimoto, H, Mild hypothermia study group in Japan., A multicenter prospective randomized controlled trial of the efficacy of mild hypothermia for severely head injured patients with low intracranial pressure. J Neurosurg, 2001. 94: p. 50-4.
289. Faber, P., Garby. L., Fat content affects heat capacity: a study in mice. Acta Physiol Scand, 1995. 153: p. 185–7.
290. Sargent , J., Seffl, RJ., Properties of perfluorinated liquids. Fed Proc, 1970. 29: p. 1699-1703.
291. Simmons, J., Fluorine chemistry, vols I, II, and V., ed. J. Simmons. 1950, New York: New York: Academic Press.
292. Riess, J.G., Le Blanc, M, Solubility and transport phenomenon in perflurochemicals relevant to blood substitution and other biomedical applications. Pure & Appl.Chem., 1982. 54(12): p. 2383-24O6.
293. Banks, R., Smart, BE, Tatlow, JC, ed. Organofluorine Chemistry: Principles and Commercial Applications. Topics in Applied Chemistry., ed. R. Banks. 1994, Plenum Press: New York and London.
294. Bondi, A., van der Waals volume and radii. J Phys Chem, 1964. 68: p. 441-450.
295. Krafft, M., Reiss, JG., Highly fluorinated amphiphiles and colloidal systems, and their applications in the biomedical field. A contribution. Biochimie. 1998. 80: p. 489-514.
296. Sargent, J.W., Seffl R J. , Properties of perfluorinated liquids. . Fed Proc 1970. 29: p. 1699-1703.
297. Lowe, K., Perfluorocarbons as oxygen-transport fluids. Comp Biochem Physiol, 1987. 87: p. 825-38.
298. Lowe, K., Fluorinated Blood Substitutes and Oxygen Carriers. J Fluorine Chem, 2001. 109: p. 59-65.
299. Riess, J., Krafft, MP., Advanced fluorocarbon-based systems for oxygen and drug delivery, and diagnosis. Artif Cells Blood Substit Immobil Biotechnol, 1997. 25: p. 43-52.
300. Schaffer, T., et al., Physiological effects of ventilation with liquid fluorocarbon at controlled temperatures. Undersea Biomed Res, 1984. 3: p. 287-98.
301. Reiss, J., Oxygen Carriers (“Blood Substitutes”)-Raison d’Etre, Chemistry, and Some Physiology Blut ist ein ganz besondrer Saft. . Chem Rev, 2001. 101: p. 2797-2920.
302. Geyer, R. Oxygen Carrying Colloidal Blood Substitutes. in Proc Internatl Symp. 1981. Munich: W. Zuckschwerdt Verlag.
303. Riess, J., Overview of progress in the fluorocarbon approach to in vivo oxygen delivery. Biomater Artif Cells Immobilization Biotechnol, 1992. 20: p. 183-202.
304. Jeng, M., et al., Perfluorochemical (PFC) Combinations for Acute Lung Injury: An In Vitro and In Vivo Study in Juvenile Rabbits. Pediatr Res, 2003. 53: p. 81-88.
305. Nagase, S., Banks, RE., Preparation, properties, and industrial applications of organofluorine compounds., R. Banks, Editor. 1982, Ellis Horwood Ltd; Halsted Press: Chichester West Sussex and New York.
306. Singh, R., Shreeve JM., Perfluoroalkylation of simple inorganic molecules: A one step route to novel perfluoroalkylated compounds. Chem Commun, 2002. 7: p. 1818 – 1819.
307. Conte, L., Napoli, M, Gambaretto, GP., J. Fluorine Chem, 1985. 30: p. 89.
308. Shaffer, T., et al., Liquid ventilation. Pediatr Pulmonol, 1992. 14: p. 102-9.
309. Clark, L., Jr, Hoffmann, RE, Davis, SL., Response of the rabbit lung as a criterion of safety for fluorocarbon breathing and blood substitutes. Biomater Artif Cells Immobilization Biotechnol, 1992. 20(2-4): p. 1085-99.
310. Lattes, A., Rico-Lattes, I., Microemulsions of perfluorinated and semi-fluorinated compounds. Artif Cells Blood Substit Immobil Biotechnol, 1994. 22(4): p. 1007-18.
311. Chubb, C., Reversal of the endocrine toxicity of commercially produced perfluorochemical emulsion. Biol Reprod, 1985. 33: p. 854-58.
312. 3-M-Company, 3M Fluorinert liquids for electronic manufacturing: publication 4658 (HB)98-0212-3713-03. 2003: 3M Company, St, Paul, MN.
313. Kaisers, U., K.P. Kelly, and T. Busch, Liquid ventilation. Br J Anaesth, 2003. 91(1): p. 143-51.
314. Sass, D., Van Dyke, RA, Wood, EH, Johnson, SA, Didisheim, P., Gas embolism due to intravenous FC 80 liquid fluorocarbon. J Appl Physiol, 1976. 40(5): p. 745-51.
315. Leakakos, T., Schutt, EG, Cavin, JC, Smith, D, Bradley, JD, Strnat, DA, del Balzo, U, Hazard, DY, Otto, S, Fields, TK, et al., Pulmonary gas trapping differences among animal species in response to intravenous infusion of perfluorocarbon emulsions. Artif Cells Blood Substit Immobil Biotechnol, 1994. 22: p. 1199-204.
316. Schutt, E., Barber, P, Fields, T, Flaim, S, Horodniak, J, Keipert, P, Kinner, R, Kornbrust, L, Leakakos, T, Pelura, T, et al., Proposed mechanism of pulmonary gas trapping (PGT) following intravenous perfluorocarbon emulsion administration. Artif Cells Blood Substit Immobil Biotechnol, 1994. 22: p. 1205-14.
317. Burns, M.J., et al., Enhanced mortality from perfluorocarbon administration in a rat model of kerosene aspiration. J Toxicol Clin Toxicol, 1999. 37: p. 855-9.
318. Mason, K., Withers, HR, Steckel, RJ., Acute effects of a perfluorochemical oxygen carrier on normal tissues of the mouse. Radiat Res, 1985. 104: p. 387-94.
319. Bucala, R., Kawakami, M, Cerami, A., Cytotoxicity of a perfluorocarbon blood substitute to macrophages in vitro. Science, 1983. 27: p. 965-7.
320. Edwards, C., Lowe, KC, Röhlke, W, Geister, U, Reuter, P, Meinert , H., Effects of a novel perfluorocarbon emulsion on neutrophil chemiluminescence in human whole blood in vitro. Artif Cells Blood Substit Immobil Biotechnol, 1997. 25: p. 255-60.
321. Flaim, S., Pharmacokinetics and side effects of perfluorocarbon-based blood substitutes. Artif Cells Blood Substit Immobil Biotechnol, 1994. 22: p. 1043-54.
322. Wiedemann, H., Partial liquid ventilation for acute respiratory distress syndrome. Clin Chest Med,, 2000. 21: p. 543-54.
323. Augustin, A., Spitznas, M, Koch, FH, Böker, T, Meller D, Lutz J., Systemic effects of different perfluorochemical agents. Graefes Arch Clin Exp Ophthalmol, 1995. 233: p. 48-51.
324. van Eeden, S., Klut, ME, Leal, MA, Alexander, J, Zonis, Z, Skippen, P., Partial liquid ventilation with perfluorocarbon in acute lung injury: light and transmission electron microscopy studies. Am J Respir Cell Mol Biol, 2000. 22: p. 441-50.
325. Koch, T., et al., Perfluorohexane attenuates proinflammatory and procoagulatory response of activated monocytes and alveolar macrophages. Anesthesiology, 2001. 94(1): p. 101-9.
326. Rotta, A., Steinhorn, DM., Partial liquid ventilation reduces pulmonary neutrophil accumulation in an experimental model of systemic endotoxemia and acute lung injury. Crit Care Med, 1998. 26(10): p. 1707-15.
327. Wada, S., Kajihara, H, Murakami, H, Sueda, T, Matsuura ,Y., Effects of FC43 emulsion against hyperacute rejection in rodent discordant xenotransplantation. Heart Lung Transplant, 1995. 14: p. 968-72.
328. Tanaka, M., [Mechanisms of rejection in guinea pig (GP)-to-rat liver xenotransplantation: improvement of recoloration of GP liver graft and effects of perfluorochemical (FC43) in GP-to-rat liver xenotransplantation][Article in Japanese]. Hokkaido Igaku Zasshi, 1999. 74: p. 441-55.
329. Gale, S.C., Gorman, G D, Copeland, J G, McDonagh, P F., Perflubron emulsion prevents PMN activation and improves myocardial functional recovery after cold ischemia and reperfusion. J Surg Res, 2007. 138: p. 135-40.
330. Cicerone, R.J., Atmospheric Carbon Tetrafluoride: A nearly Inert Gas. Science, 1979. 206: p. 59-60.
331. Yi-Tang, Atmospheric Fate of Various Fluorochemicals. 1993, Massachusetts Institute of Technology Department of Chemistry: Boston.
332. 3M-Company, 3M Fluorinert liquids for electronic manufacturing: publication 4658 (HB)98-0212-3713-03. 2003.
333. 3-M-Company, Century of Innovation: The 3M Story. 2003.
334. Renner, R., Piecing Together the Perfluroniated Puzzle. Analytical Chemistry News, 2003: p. 1A-40A.
335. Houde, M., et al., Biological monitoring of polyfluoroalkyl substances: A review. Environ Sci Technol. 2006. 40: p. 3463-73.
336. Kannan, K., et al., Perfluorooctanesulfonate and related fluorochemicals in human blood from several countries. Environ Sci Technol, 2004. 38(17): p. 4489-95.
337. Guruge, K.S., et al., Perfluorinated organic compounds in human blood serum and seminal plasma: a study of urban and rural tea worker populations in Sri Lanka. J Environ Monit, 2005. 7: p. 371-7.
338. Giesy, J.P. and K. Kannan, Global distribution of perfluorooctane sulfonate in wildlife. Environ Sci Technol, 2001. 35(7): p. 1339-42.
339. Tomy, G., Wski, W, Halldorson, T, Helmm P, Stern, G, Tittlemier, S., Fluorinated organic compounds in an eastern arctic marine food web. Organohalogen Compounds, 2003: p. 323-327.
340. Tao, L., et al., Perfluorooctanesulfonate and related fluorochemicals in albatrosses, elephant seals, penguins, and polar skuas from the Southern Ocean. Environ Sci Technol, 2006. 40(24): p. 7642-8.
341. Brown, D., Mayer , CE. and 3M to pare Scotchgard products: one long-lasting compound is cited., in The Washington Post. May 17, 2000. 2000: Washington, D.C.
342. Fromme, H., et al., Occurrence of perfluorinated substances in an adult German population in southern Bavaria. Int Arch Occup Environ Health, 2007. 80(4): p. 313-9.
343. Calafat, A., Needham, LL, Kuklenyik, Z, Reidy, JA, Tully, JS, Aguilar-Villalobos, M, Naeher, LP., Perfluorinated chemicals in selected residents of the American continent. Chemosphere, 2006. 63(3): p. 490-6.
344. Kudo, N., Kawashima, Y., Toxicity and toxicokinetics of perfluorooctanoic acid in humans and animals. J Toxicol Sci, 2003. 28(2): p. 49-57.
345. Nakayama, S., Harada, K, Inoue, K, Sasaki, K, Seery, B, Saito, N, Koizumi, A., Distributions of perfluorooctanoic acid (PFOA) and perfluorooctane sulfonate (PFOS) in Japan and their toxicities. Environ Sci, 2005. 12(6): p. 293-313.
346. Karrman, A., et al., Levels of 12 perfluorinated chemicals in pooled australian serum, collected 2002-2003, in relation to age, gender, and region. . Environ Sci Technol, 2006. 40: p. 3742-8.
347. Kudo, N. and Y. Kawashima, Toxicity and toxicokinetics of perfluorooctanoic acid in humans and animals. J Toxicol Sci, 2003. 28(2): p. 49-57.
348. Yang, Q., et al., Potent suppression of the adaptive immune response in mice upon dietary exposure to the potent peroxisome proliferator, perfluorooctanoic acid. Int Immunopharmacol, 2002. 2(2-3): p. 389-97.
349. Yang, Q., et al., Involvement of the peroxisome proliferator-activated receptor alpha in the immunomodulation caused by peroxisome proliferators in mice. Biochem Pharmacol, 2002. 63(10): p. 1893-900.
350. Peden-Adams, M.M., et al., Suppression of humoral immunity in mice following exposure to perfluorooctane sulfonate. Toxicol Sci, 2008. 104(1): p. 144-54.
351. Kannan, K., Perrotta, E, Thomas, NJ., Association between perfluorinated compounds and pathological conditions in southern sea otters. Environ Sci Technol, 2006. 40(16): p. 4943-8.
352. Bagwell, C., Ambroise Pare and the renaissance of surgery. Surg Gynecol Obstet, 1981. 152: p. 350-5.
353. Dosey, B., Florence Nightingale: Mystic, Visionary, Healer. 2000, New York: Lippincott Williams & Wilkins.
354. Cannon, W., Traumatic Shock. 1923, New York: Appleton Company, Inc.
355. Blalock, A., Principles of Surgical Care: Shock and Other Problems. 1940, St. Louis: Mosby.
356. Parrish, T., The Submarine: A History. 2005, New York: Penguin.
357. Klystra, J., Lavage of the lung. Acta Physiol Pharmacol Neerl, 1958. 7: p. 163-221.
358. Klystra, J., Simplified technique of lavage of the lung. Acta Physiol Pharmacol Neerl, 1960. 9: p. 225-39.
359. Klystra, J., Breathing of pressure oxygenated salt solutions. Chest, 1965. 47: p. 157.
360. Klystra, J., et al., Lavage of the lung. II. A report on “long term” effects in dogs and suggestions concerning possible modifications of the original technique in order to improve its applicability for the treatment of chronic progressive and fatal diseases of the kidney in man. Acta Physiol Pharmacol Neerl., 1959. 8: p. 326-36.
361. Costa, E., Amato, M., Maintenance of end-expiratory recruitment with increased respiratory rate after saline-lavage lung injury. J Appl Physiol, 2007. 102: p. 2414.
362. Brederlsau, J., et al., Combination of arteriovenous extracorporeal lung assist and high-frequency oscillatory ventilation in a porcine model of lavage-induced acute lung injury: a randomized controlled trial. J Trauma, 2007. 62: p. 336-46; discussion 345-6.
363. Klystra, J., Schoenfisch, X, Maximum expiratory flow and estimated CO2 elimination in liquid-ventilated dogs’ lungs. J. Appl Physiol 1973. 35: p. 117-121.
364. Clark, L., Introduction to federation proceedings. Fed Proc, 1970. 29: p. 698.
365. Moskowitz, G., A mechanical respirator for control of liquid breathing. Fed Proc, 1970. 29: p. 1751-2.
366. Moskowitz, G., et al., Liquid breathing trials and animal studies with a demand-regulated breathing system. Med Instrum, 1975. 9: p. 28-33.
367. Shaffer, T., Moskowitz, GD., An electromechanical demand regulated liquid breathing system. IEEE Trans Biomed Eng, 1975. 22: p. 24-8.
368. Shaffer, T., Moskowitz, GD., Demand-controlled liquid ventilation of the lungs. J Appl Physiol, 1974. 36: p. 208-13.
369. Schaffer, T., et al., The effects of liquid ventilation on cardiopulmonary function in pre-term lambs. Pediatr Res, 1983. 17: p. 303.
370. Greenspan, J., et al., Liquid ventilation of a preterm baby. Lancet, 1989. 2: p. 1095.
371. Shaffer, T.H., Moskowitz, G D., Demand-controlled liquid ventilation of the lungs. J Appl Physiol, 1974. 36: p. 208-13.
372. Furhman, B., et al., Perfluorocarbon-associated gas exchange. Crit Care Med., 1991. 19: p. 712-22.
373. Marraro, G., Bonati, M, Ferrari, A, Barzaghi, MM, Pagani, C, Bortolotti, A, Galbiati, A, Luchetti, M, Croce, A., Perfluorocarbon broncho-alveolar lavage and liquid ventilation versus saline broncho-alveolar lavage in adult guinea pig experimental model of meconium inhalation. Intensive Care Med, 1998. 24(5): p. 501-8.
374. Bull, J., et al., Flow limitation in liquid-filled lungs: effects of liquid properties. J Biomech Eng, 2005. 127: p. 630-6.
375. Suresh, V., Anderson, JC, Grotberg, JB, Hirschl, RB., A mathematical model of alveolar gas exchange in partial liquid ventilation. J Biomech Eng, 2005. 127(1): p. 46-59.
376. Sekins, K., et al., Long-term partial liquid ventilation (PLV) with perflubron in the near-term baboon neonate. Artif Cells Blood Substit Immobil Biotechnol, 1994. 22: p. 1381-7.
377. Foust, R., 3rd, et al., Liquid assisted ventilation: an alternative ventilatory strategy for acute meconium aspiration injury. Pediatr Pulmonol, 1996. 21: p. 316-22.
378. Momoki, Y., et al., Experimental study in partial liquid ventilation for acute respiratory failure after ischemia reperfusion pulmonary injury in a rabbit model. Jpn J Thorac Cardiovasc Surg., 1998. 46: p. 65-70.
379. Dickson, E., et al., Partial liquid ventilation with perfluorocarbon in the treatment of rats with lethal pneumococcal pneumonia. Anesthesiology, 1998. 88: p. 218-23.
380. Younger, J., et al., Partial liquid ventilation protects lung during resuscitation from shock. Appl Physiol, 1997. 83: p. 666-70.
381. Verbrugge, S., et al., Different ventilation strategies affect lung function but do not increase tumor necrosis factor-alpha and prostacyclin production in lavaged rat lungs in vivo. Anesthesiology, 1999. 91: p. 1834-43.
382. Arnold, J., et al., Prospective, randomized comparison of high-frequency oscillatory ventilation and conventional mechanical ventilation in pediatric respiratory failure. Crit Care Med, 1994. 22: p. 1530-39.
383. Hirschl, R., Liquid ventilation in the setting of respiratory failure. Asaio J, 1998. 44(3): p. 231-3.
384. Kacmarekm RM, L., PT, et al., Partial liquid ventilation in adult patients with acute respiratory distress syndrome. Am J Respir Crit Care Med, 2006. 178: p. 882-89.
385. Lemaire, F., Low- dose perfluorocarbon: A revival for partial liquid ventilation? Crit Care Med, 2007. 35: p. 662-63.
386. Pound, P., et al., Where is the evidence that animal research benefits humans? BMJ, 2004. 328: p. 514.
387. ARDSnet, Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volume as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Eng J Med, 2000. 342: p. 1301-08.
388. ARDSnet, Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. NEM, 2000. 342: p. 1301-08.
389. Lim, C.M., et al., An optimal dose of perfluorocarbon for respiratory mechanics in partial liquid ventilation for dependent lung-dominant acute lung injury. Chest, 2000. 117: p. 199-204.
390. Tutuncu, A., et al., Intratracheal perfluorocarbon administration as an aid in the ventilatory management of respiratory distress syndrome. Anesthesiology, 1993. 79: p. 1083-93.
391. Ricard, J., et al., Perflubron™ dosing affects ventilator-induced lung injury in rats with previous lung injury. Crit Care Med, 2007. 35: p. 561-67.
392. Ricard, J.D., et al., Perflubron dosing affects ventilator-induced lung injury in rats with previous lung injury. Crit Care Med, 2007. 35(2): p. 561-7.
393. Ricard, J., Dreyfuss, D, Laissy, J. P., et al., Dose-response effect of perfluorocarbon administration on lung microvascular permeability in rats. Am J Respir Crit Care Med, 2003. 168: p. 1378-82.
394. Tredici, S., Tredici, F, Brant, DO, Hirschl, RB, Bull, JL., Effect of viscosity on instilled perfluorocarbon distribution in rabbit lungs. J Biomech Eng, 2006. 128: p. 857-61.
395. Zheng, Y., et al., Effects of inertia and gravity on liquid plug splitting at a bifurcation. J Biomech Eng, 2006. 128(5): p. 707-16.
396. Hirschl, R., et al., Prospective, randomized, controlled pilot study of partial liquid ventilation in adult acute respiratory distress syndrome. Crit Care Med, 2002. 165: p. 781-87.
397. Wiedemann, H., et al., A multicenter, randomized, feasibilitystudy of two doses of perflubron administered for partial liquid ventilation in patients with acute respiratory distress syndrome. Abstr. Am J Respir Crit Care Med, 1999. 159:A80.
398. Griese, M., Griese M. Pulmonary surfactant in health and human lung diseases: state of the art. Eur Respir J, 1999. 13: p. 1455-76.
399. Rosenzweig, J., Jensen, OE., Capillary-elastic instabilities of liquid-lined lung airways. J Biomech Eng, 2002. 124(6): p. 650-55.
400. Kamm, R., Schroter, RC., Is airway closure caused by a liquid film instability? Respir Physiol, 1989. 75(2): p. 141-56.
401. Salman, N., Fuhrman, BP, Steinhorn, DM, et al., Prolonged studies of perfluorocarbon-associated gas exchange and of the resumption of conventional mechanical ventilation. Crit Care Med, 1995. 23: p. 919-24.
402. Kaisers, U., et al., Partial liquid ventilation with small volumes of FC 3280 increases survival time in experimental ARDS. Eur Respir J 1997. 10.
403. West, J., Tsukimoto K, Mathieu-Costello, O, et al., Stress failure in pulmonary capillaries. J Appl Physiol, 1991. 70: p. 1731-42.
404. Dos Santos, C., Slutsky, AS., Invited review: Mechanisms of ventilator-induced lung injury: a perspective. J Appl Physiol, 2000. 89: p. 1645-1655.
405. Chu, E., Whitehead, T, Slutsky, AS., Effects of cyclic opening and closing at low- and high-volume ventilation on bronchoalveolar lavage cytokines. Crit Care Med, 2004. 32: p. 168-74.
406. Dreyfuss, D., Saumon, G, Ventilator-induced lung injury: Lessons from experimental studies. Am J Respir Crit Care Med, 1998. 157: p. 294-323.
407. Hughes, J., Rosenzweig, DY, Kivitz, PB., Site of airway closure in excised dog lungs: histological demonstration. J Appl Physiol, 1970. 29: p. 340-344.
408. Ghadiali, S.N. and D.P. Gaver, Biomechanics of liquid-epithelium interactions in pulmonary airways. Respir Physiol Neurobiol, 2008. 163(1-3): p. 232-43.
409. Argiras, E., Blakeley, CR, Dunnill, MS, Otremski, S, Sykes, MK., High PEEP decreases hyaline membrane formation in surfactant deficient lungs. Br J Anaesth 1987. 59: p. 1278-1285.
410. Gaver, D., Halpern, D, III, Jensen, O, Grotberg, JB., The steady motion of a semi-infinite bubble through a flexible-walled channel. J Fluid Mech, 1996. 319: p. 25-65.
411. Mead, J., Takishima, T, Leith, D., Stress distribution in lungs: a model of pulmonary elasticity. J Appl Physiol, 1970. 28: p. 596-608.
412. Yap, D., Gaver, D., The influence of surfactant on two-phase flow in a flexible-walled channel under bulk equilibrium conditions. Phys Fluids, 1998. 10: p. 1846-1863.
413. Bilek, A., Dee, KC, Gaver, DP, III., Mechanisms of surface-tension-induced epithelial cell damage in a model of pulmonary airway reopening. J Appl Physiol, 2003. 94: p. 770-783.
414. Naureckas, E., Dawson, CA, Gerber, BS, Gaver, DP, Gerber, HL III, Linehan, JH, Solway, J, and Samsel, RW., Airway reopening pressure in isolated rat lungs. J Appl Physiol, 1994. 76: p. 1372-1377.
415. Yap, D., Liebkemann, W, Solway, J, Gaver, D., Influences of parenchymal tethering on the reopening of closed pulmonary airways. J Appl Physiol, 1994. 76: p. 2095-2105.
416. Jensen, O., Horsburgh, MK, Halpern, D, Gaver, DP, III., The steady propagation of a bubble in a flexible-walled channel: asymptotic and computational models. Phys Fluids 2002. 14: p. 443-457.
417. Vlahakis, N., Hubmayr, RD., Invited review: plasma membrane stress failure in alveolar epithelial cells. J Appl Physiol, 2000. 89: p. 2490-2497.
418. Doctor, A., et al., High-frequency oscillatory ventilation of the perfluorocarbon-filled lung: preliminary results in an animal model of acute lung injury. Crit Care Med, 1999. 27(11): p. 2500-7.
419. Rotta, A.T., et al., Combining lung-protective strategies in experimental acute lung injury: The impact of high-frequency partial liquid ventilation. Pediatr Crit Care Med, 2006. 7(6): p. 562-70.
420. Harris, S.B., New Breakthrough in Rapid Cooling of Cryopreservation Patients after Cardiac Arrest, presented at the Suspended Animation, Inc. Advances in Cryopreservation Conference. 2007: 19 May, Ft. Lauderdale.
Appendix B: Explanation of the Mechanics of Blood Flow during Closed Chest CPR: The Thoracic Pump Theory
The following text, with the accompany references, is reproduced from Weisfeldt, M., Chandra, N., Physiology of cardiopulmonary resuscitation. Ann Rev Med, 1981. 32: p. 43-42.
“At least three general mechanisms are now thought to contribute to the generation of the extrathoracic arterial-venous pressure gradient observed during conventional CPR in the dog. These factors are (a) various venous valving mechanisms are operating, (b) peripheral venous capacitance greater than arterial capacitance, and (c) arterial resistance to collapse greater than venous resistance.
The most easily understood of these mechanisms is that of a valving mechanism. Veins at the thoracic inlet and other veins leading from the brain appear to have anatomic valves that prevent retrograde flow of blood during increases in intrathoracic pressures (9, 10, 16, 18). The valves along the extrathoracic veins, and the one at the thoracic inlet appear to be important.
The second factor contributing to the generation of the peripheral arterial-venous pressure gradient is that venous capacitance is greater than arterial. Clearly, if the same amount of blood were to move from the intrathoracic arterial and from the intrathoracic venous systems into the extrathoracic arterial and venous systems, arterial pressure would rise more than venous pressure because of the differences in extrathoracic arterial and venous capacitance.
The third contributor to the peripheral arterial-venous pressure gradient is the difference in arterial and venous resistance to collapse. Venous structures readily collapse when inside pressures fall below surrounding pressures by even a small amount. Recently we showed that the in vivo carotid artery at the thoracic inlet exhibits considerable intrinsic resistance to collapse.
This resistance to collapse can be increased in the presence of vasoconstrictor agents (23). Resistance to collapse of the arterial vessels would allow blood flow to continue toward the brain despite surrounding intrathoracic pressures which exceed intravascular pressures. The veins would readily collapse at the exit to the high pressure region, i.e. at the thoracic inlet (1, 13).
Blood returns from the periphery to the central circulation between compression cycles. Extrathoracic venous pressure rises (20) when blood flows from arteries to veins during compression. Between compressions intrathoracic pressure falls to near atmospheric, and an extrathoracic-to intrathoracic venous pressure gradient appears, which leads to flow into the chest. Right heart and pulmonary blood flow is also diastolic, at least in part (7). With conventional CPR, fight heart compression may be a component of the mechanism for pulmonary flow.”
References
1. Brecher, G. A. 1952. Mechanism of venous flow under different degrees of aspiration. Am. J. Physiol. 169-423.
7. Cohen, J. M., Alderson, P. O., Van AswegenA, ., Chandra,N ., Tsitlik, J.,
Weisfeldt,M .L . 1979.T imingo f intrathoracic blood flow during resuscitation
with high intrathoracic pressure. Circulation. 59 & 60:II-19.
10. Franklin,K . J. 1927.V alvesin veins: an historical survey. In Proc. R. Soc. ed. Sect. History Med., pp. 4-6.
13. Holt, J. P. 1941. The collapse factor in the measurement of venous pressure.
Am. J. Physiol. 134:292.
16. MacKenzie, J. 1894. The venous and liver pulses, and the arhythmie (sic) contraction of the cardiac cavities, d. Pathol. Bacteriol. 2:113.
18. Niemann, J. T., Garner, D., Rosborough, J., Criley, J. M. 1979. The mechanism of blood flow in closed chest cardiopulmonary resuscitation. Circulation 59 & 60:I1-74.
21. Weale,F . E., Rothwell-JacksonR, . L. 1962. The efficiency of cardiac massage. Lancet 1:990-92.
23. Yin, F. C. P., CohenJ,. M., Tsitlik, J., Weisfeldt, M. L. 1979. Arterial resistance
to collapse: A determinant of peripheral flow resulting from high intrathoracic
pressure. Circulation 59 & 60:I1-196.
Reproduced from the Annual Reviews www.annualreviews.org/aronline
Annu. Rev. Med. 1981.32:435-442. Downloaded from: arjournals.annualreviews.org by PALCI on 10/25/08.

 “Really?” I replied with some skepticism.
“Really?” I replied with some skepticism. As it turned out, she became a sensation, went onto fame in the U.S., sold millions of albums! It was mad, absolutely mad! And I assure you, it had nothing to do with her raw talent. She was one of millions and millions of would-be nucleating agents trying for that peculiar niche, and she was in exactly the right place at exactly the right time. Did she think she was going to be a multimillionaire hit recording star? It doesn’t really matter, because she is. It’s very much like the lottery if you are poor , disenfranchised, have no other options and desperately want to get hold of millions. Well it’s really your only chance, and if you don’t play, you can’t win.
As it turned out, she became a sensation, went onto fame in the U.S., sold millions of albums! It was mad, absolutely mad! And I assure you, it had nothing to do with her raw talent. She was one of millions and millions of would-be nucleating agents trying for that peculiar niche, and she was in exactly the right place at exactly the right time. Did she think she was going to be a multimillionaire hit recording star? It doesn’t really matter, because she is. It’s very much like the lottery if you are poor , disenfranchised, have no other options and desperately want to get hold of millions. Well it’s really your only chance, and if you don’t play, you can’t win. “Like Dr. Arthur Rowe, who, in fact, is still alive, and recently, like a frozen Woolly Mammoth in some bad B-movie, has come back to life, eons later, and is making TV appearances again, trashing cryonics.”
“Like Dr. Arthur Rowe, who, in fact, is still alive, and recently, like a frozen Woolly Mammoth in some bad B-movie, has come back to life, eons later, and is making TV appearances again, trashing cryonics.” I was stunned. Frankly, I was more stunned than I am today, having just been informed that both my parents have been dead for four months and that I was deliberately not informed about it. It shook me to core. I realized, as I read over that traffic, that cryonics was in no way going to work. It wasn’t an opinion, or a guess, or a hunch, it was a simple fact. It was like turning on the TV on 9/11 and seeing those people falling from one of the Twin Towers. There could be absolutely no question in your mind that whilst those people were alive, they were absolutely certain to be dead within a (short) and quantifiable period of time.
I was stunned. Frankly, I was more stunned than I am today, having just been informed that both my parents have been dead for four months and that I was deliberately not informed about it. It shook me to core. I realized, as I read over that traffic, that cryonics was in no way going to work. It wasn’t an opinion, or a guess, or a hunch, it was a simple fact. It was like turning on the TV on 9/11 and seeing those people falling from one of the Twin Towers. There could be absolutely no question in your mind that whilst those people were alive, they were absolutely certain to be dead within a (short) and quantifiable period of time.


 Me at the Cryonics Society of New York in the summer of 1972.
Me at the Cryonics Society of New York in the summer of 1972. Me freezing “dead” people in 1973 at age 17.
Me freezing “dead” people in 1973 at age 17. My parents gave me a great childhood. They offered me every opportunity for education and personal growth any boy could want and as only child they and I had the economic opportunity for both toys in an abundance that many children in larger families don’t enjoy. I’d like to think that both they and I took full advantage of that opportunity.
My parents gave me a great childhood. They offered me every opportunity for education and personal growth any boy could want and as only child they and I had the economic opportunity for both toys in an abundance that many children in larger families don’t enjoy. I’d like to think that both they and I took full advantage of that opportunity.


 In his 1965
In his 1965 


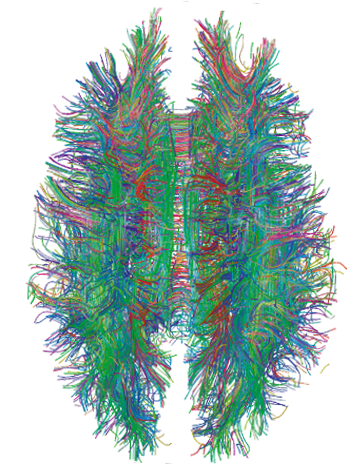
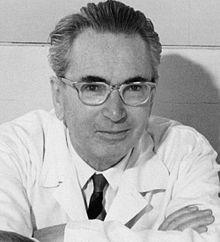
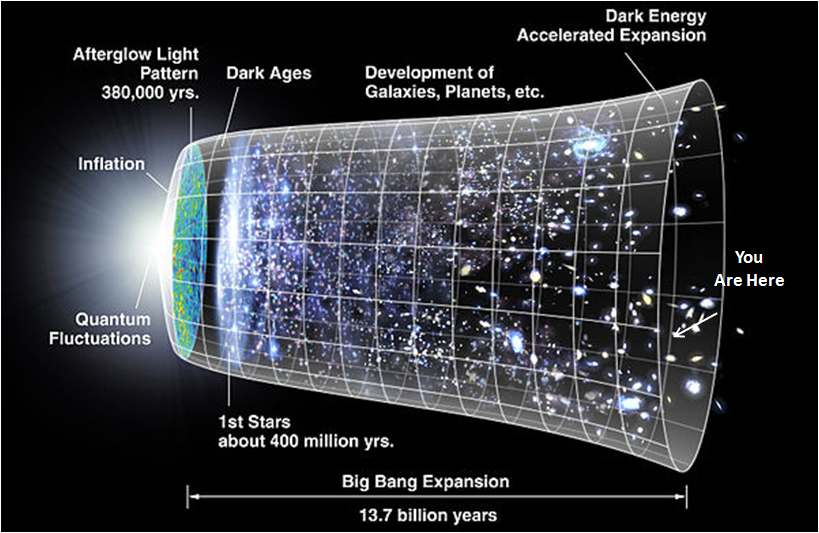
 Medicine, the law, other professions, and even academia, the trades and trade unions have such value-driven enforcement mechanisms in place. In all these examples, senior and respected members of the profession, trade, or ideological movement
Medicine, the law, other professions, and even academia, the trades and trade unions have such value-driven enforcement mechanisms in place. In all these examples, senior and respected members of the profession, trade, or ideological movement
 This is most evident in the case of Alcor, where the proof of such a standard-less or “lawless” operation can be found in the high turnover of management and staff.
This is most evident in the case of Alcor, where the proof of such a standard-less or “lawless” operation can be found in the high turnover of management and staff. Even where there are standards that are well known and written down (somewhere), such as the conditions under which at-need cases should be accepted, they are violated (as in the case of Ted Williams) – usually because those making the decisions had no mentoring and no inculturation in such rules. People do not learn “right” or “proper” behavior by being once “told the rules,” or by being given a stack of papers where they are written down (or engraved on stone, for that matter); any more than they learn moral or ethical behavior in daily life in that fashion. Such behavior, and the values that underlie them, are inculcated more than educated. No one even learns the mechanics of driving a car from reading the state-provided operator’s manual – sans lots of practice and mentoring during the actual business of operating a motor vehicle. And this is doubly true for the large body of mostly unwritten behavior that constitutes being a courteous driver! That can only be acquired from mentoring and from repetition and observation of the good conduct of others who are vastly more experienced, and for whom there is genuine respect.
Even where there are standards that are well known and written down (somewhere), such as the conditions under which at-need cases should be accepted, they are violated (as in the case of Ted Williams) – usually because those making the decisions had no mentoring and no inculturation in such rules. People do not learn “right” or “proper” behavior by being once “told the rules,” or by being given a stack of papers where they are written down (or engraved on stone, for that matter); any more than they learn moral or ethical behavior in daily life in that fashion. Such behavior, and the values that underlie them, are inculcated more than educated. No one even learns the mechanics of driving a car from reading the state-provided operator’s manual – sans lots of practice and mentoring during the actual business of operating a motor vehicle. And this is doubly true for the large body of mostly unwritten behavior that constitutes being a courteous driver! That can only be acquired from mentoring and from repetition and observation of the good conduct of others who are vastly more experienced, and for whom there is genuine respect.
 We have a profound responsibility to arrive at a world view, a morality and code of conduct of for cryonics. That these should be reasonably inclusive and flexible there can be no doubt.
We have a profound responsibility to arrive at a world view, a morality and code of conduct of for cryonics. That these should be reasonably inclusive and flexible there can be no doubt.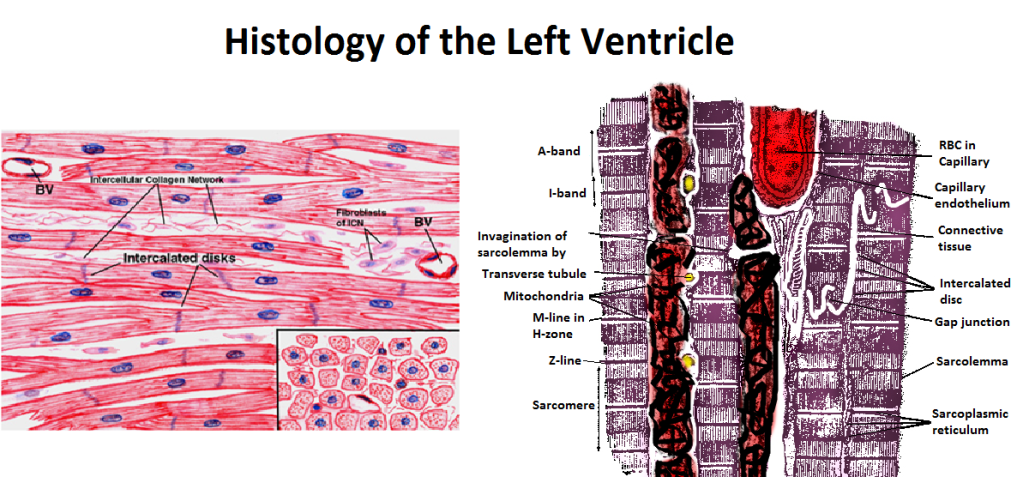 Figure 43: The myofibrils of each cardiac muscle cell are branched and contain a single nucleus. The branches interlock with those of adjacent fibers by adherens junctions which act to prevent scission of the cardiomycytes during the high-shear, forceful contractions of the heart. The muscle is richly supplied with mitochondria which are largely confined to the spaces between the fibrils. The fibrils are covered with a membrane, the Sarcolemma, which is frequently invaginated to form the Transverse tubules. These invaginations of the plasma membrane or sarcolemma, are called transverse tubules and they reach deep into the myofibrils and bring the action potential deep into the fibers. Specialized intercellular junctions, the Intercalated discs, facilitate rapid transmission of the electrical signals which initiate myocyte contraction. The myofibrils are formed by myosin and actin fibers aligned in a distinct pattern which is visible under light microscopy as the A-, H- and I- bands.
Figure 43: The myofibrils of each cardiac muscle cell are branched and contain a single nucleus. The branches interlock with those of adjacent fibers by adherens junctions which act to prevent scission of the cardiomycytes during the high-shear, forceful contractions of the heart. The muscle is richly supplied with mitochondria which are largely confined to the spaces between the fibrils. The fibrils are covered with a membrane, the Sarcolemma, which is frequently invaginated to form the Transverse tubules. These invaginations of the plasma membrane or sarcolemma, are called transverse tubules and they reach deep into the myofibrils and bring the action potential deep into the fibers. Specialized intercellular junctions, the Intercalated discs, facilitate rapid transmission of the electrical signals which initiate myocyte contraction. The myofibrils are formed by myosin and actin fibers aligned in a distinct pattern which is visible under light microscopy as the A-, H- and I- bands.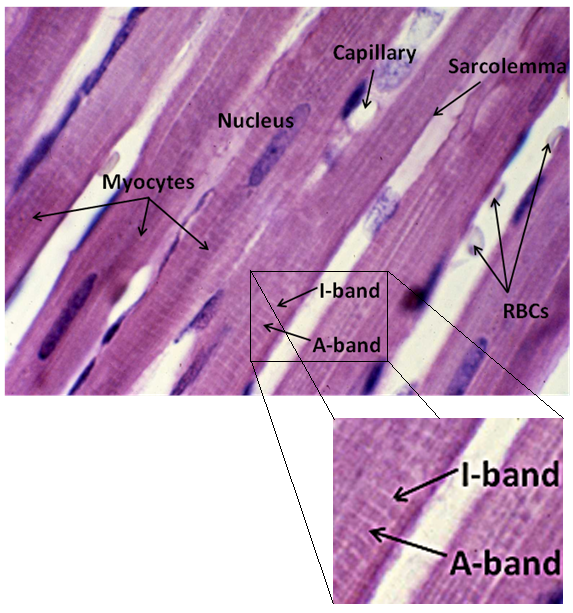
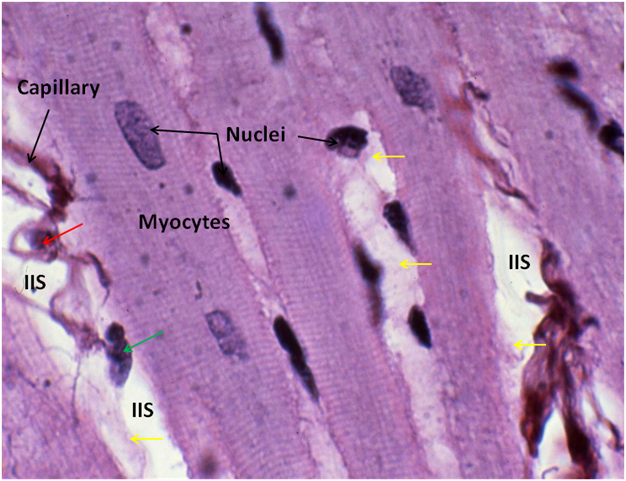
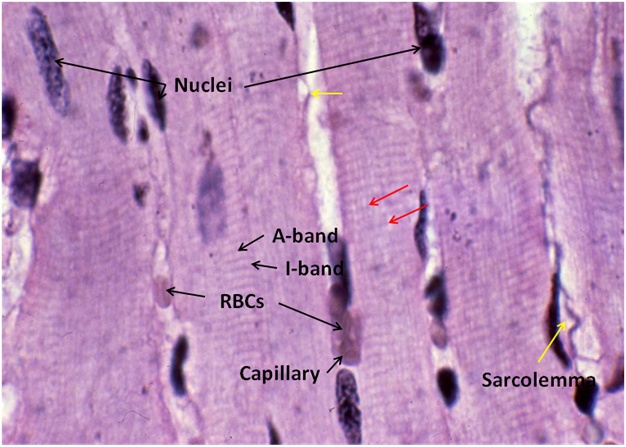
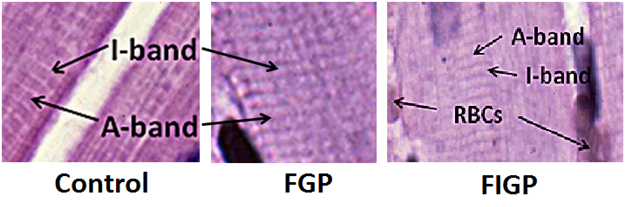
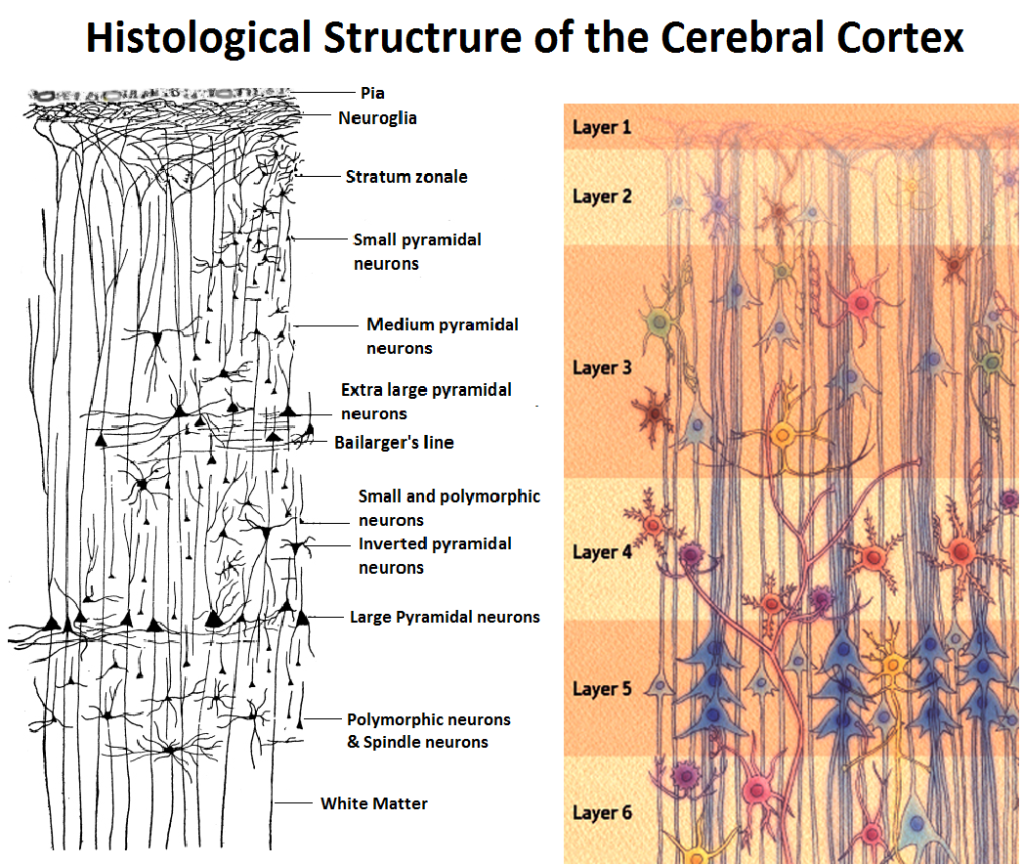 Figure 48: The cerebral cortex consists of six distinct layers, beginning with the first layer, the Molecular Layer (Stratum zonale), which consists of finely branched medullated and non-medullated nerve fibers. The molecular layer is largely devoid of neuronal cell bodies. Those neuronal cell bodies which are present are the cells of Cajal which possess irregular cell bodies and typically have four or five dendrite that terminate within the molecular layer and a long nerve fiber process, or neuraxon, which runs parallel to the surface of the cortical convolutions.
Figure 48: The cerebral cortex consists of six distinct layers, beginning with the first layer, the Molecular Layer (Stratum zonale), which consists of finely branched medullated and non-medullated nerve fibers. The molecular layer is largely devoid of neuronal cell bodies. Those neuronal cell bodies which are present are the cells of Cajal which possess irregular cell bodies and typically have four or five dendrite that terminate within the molecular layer and a long nerve fiber process, or neuraxon, which runs parallel to the surface of the cortical convolutions.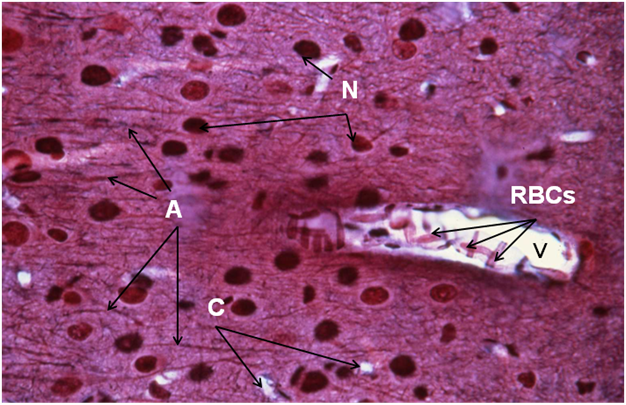
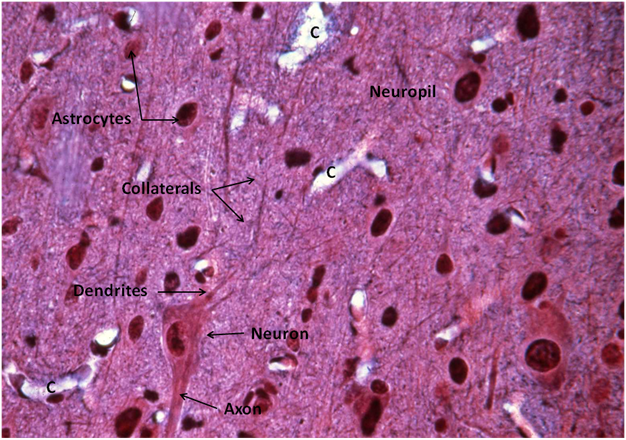
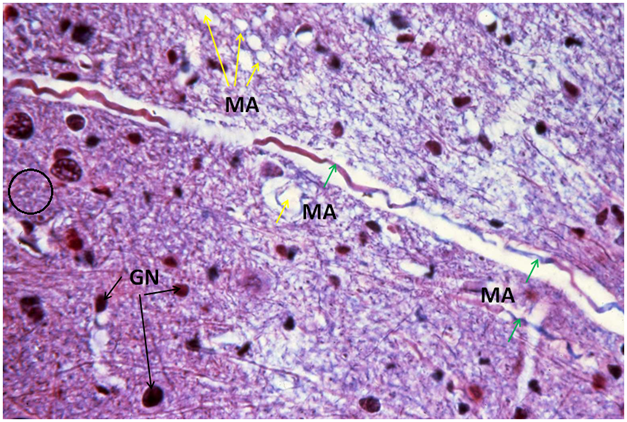
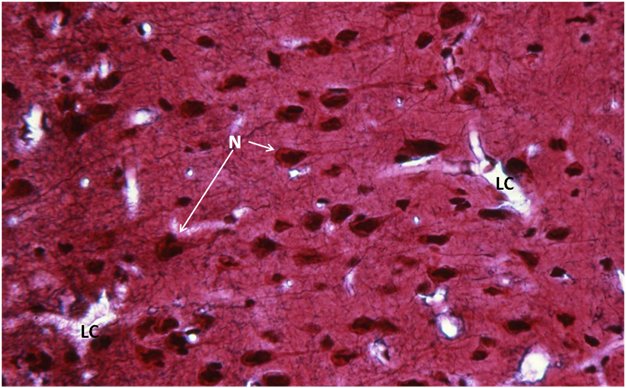
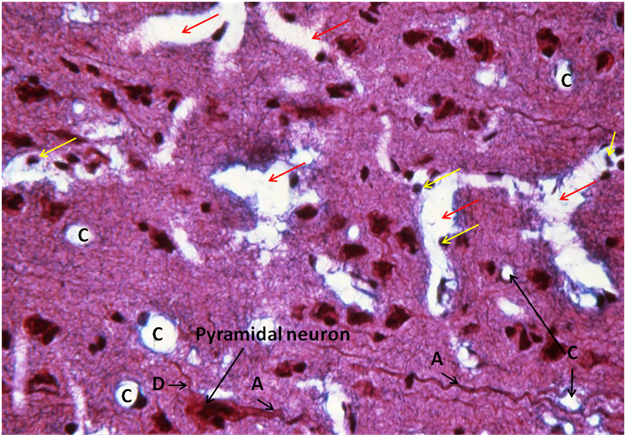
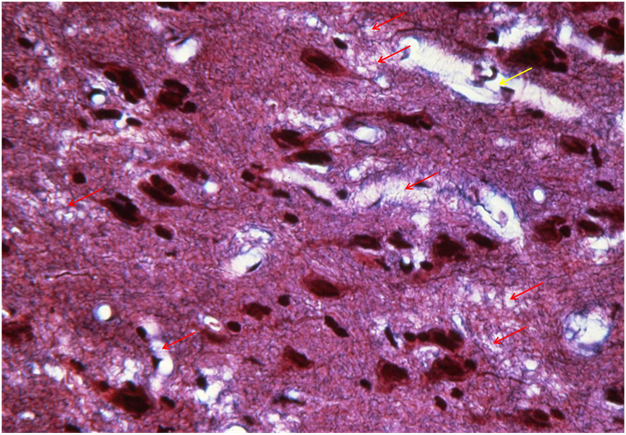
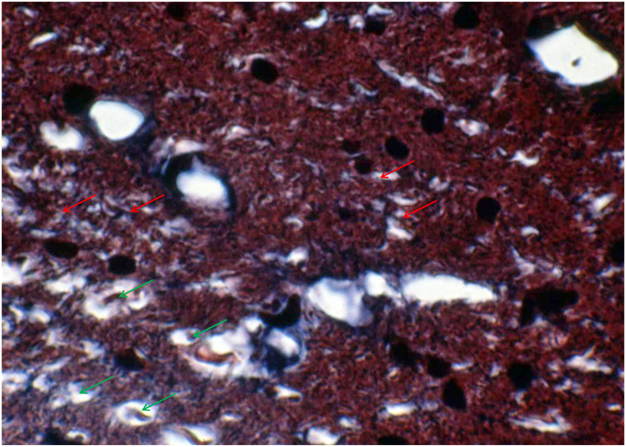
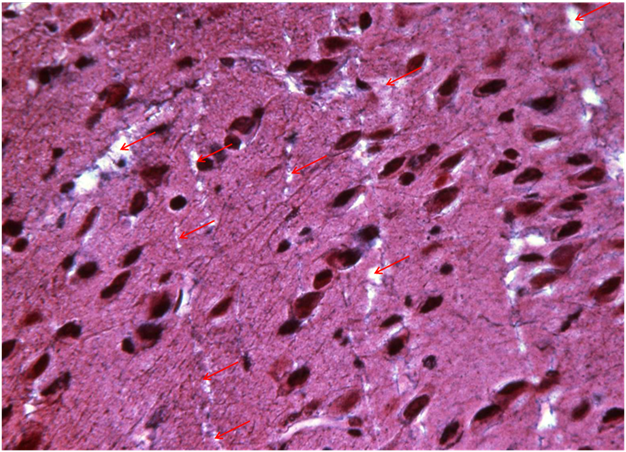
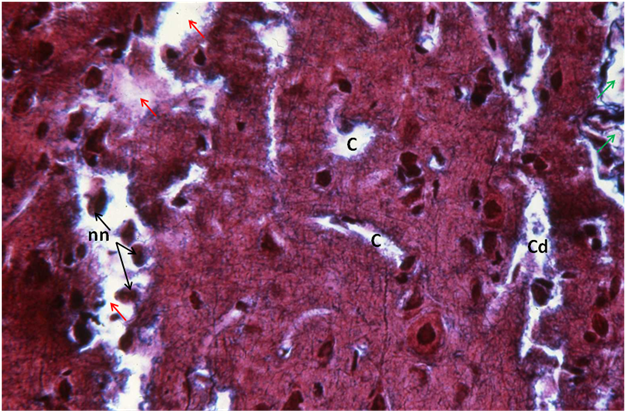
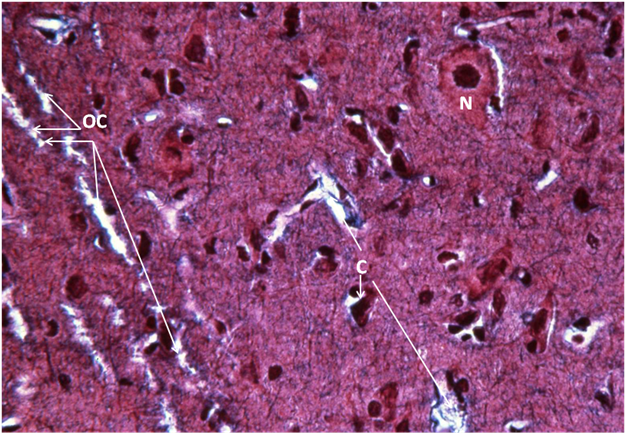
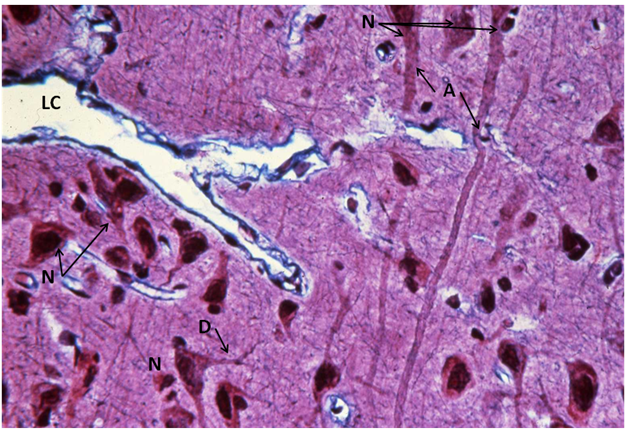
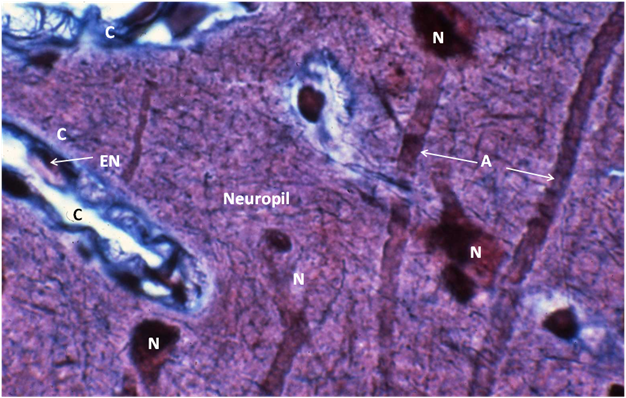
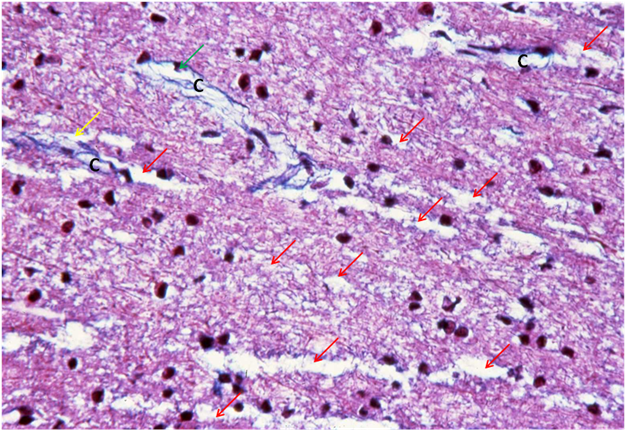












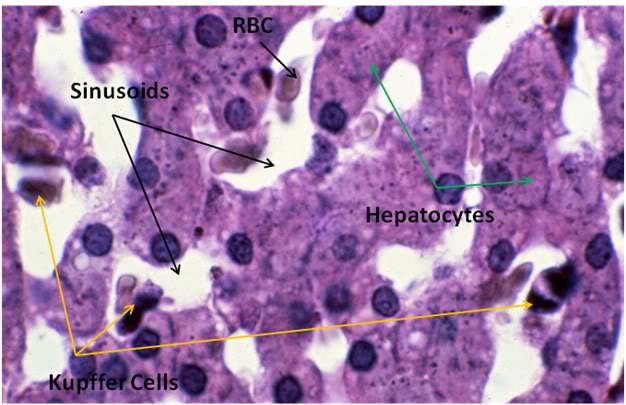 Figure 28: Control-1 Liver, Yajima, 100x. Liver sections from the Control animal demonstrated normal morphology as can be seen in the image above.
Figure 28: Control-1 Liver, Yajima, 100x. Liver sections from the Control animal demonstrated normal morphology as can be seen in the image above.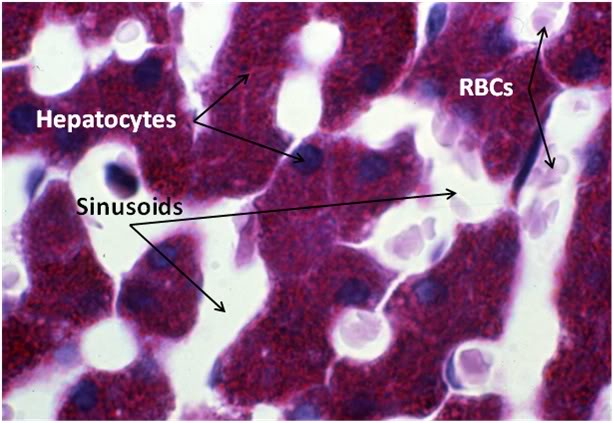
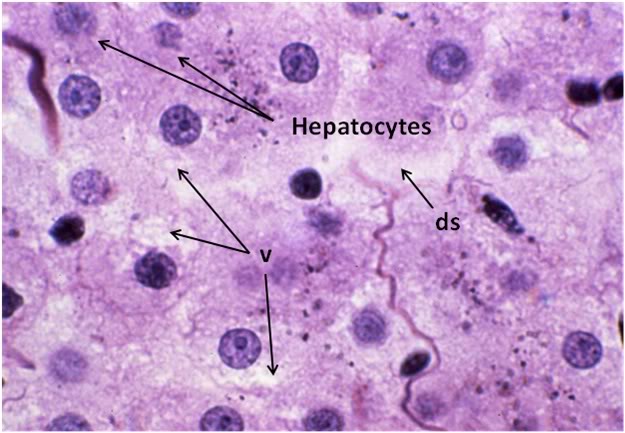 Figure 30: FGP-1 Liver, Yajima, 100x. The livers of FGP animals demonstrated extensive histological disruption. The sinusoids were all but obliterated and appeared filled with debris (ds) and the cytoplasm was extensively vacuolated (v).
Figure 30: FGP-1 Liver, Yajima, 100x. The livers of FGP animals demonstrated extensive histological disruption. The sinusoids were all but obliterated and appeared filled with debris (ds) and the cytoplasm was extensively vacuolated (v). 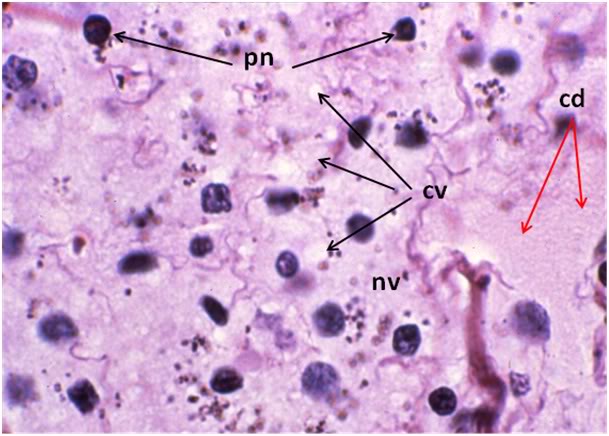 Figure 31: FIG-2 Liver, Yajima, 100x. As was the case with the FGP animals, the sinusoids were barely discernable and appeared filled with cellular debris (cd). In addition to extensive cytoplasmic (cv) and nuclear vacuolization (nv), pyknotic nuclei (pn) were also present. Cell membranes were difficult to discern and in many areas, frank cell lysis appears to have occurred with flocculent cellular debris (cd) appearing to fill the sinusoids.
Figure 31: FIG-2 Liver, Yajima, 100x. As was the case with the FGP animals, the sinusoids were barely discernable and appeared filled with cellular debris (cd). In addition to extensive cytoplasmic (cv) and nuclear vacuolization (nv), pyknotic nuclei (pn) were also present. Cell membranes were difficult to discern and in many areas, frank cell lysis appears to have occurred with flocculent cellular debris (cd) appearing to fill the sinusoids.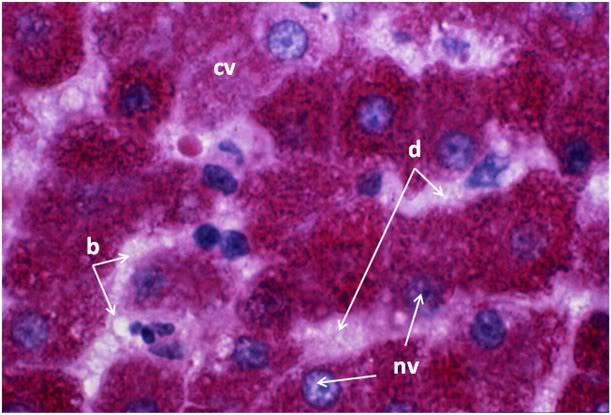 Figure 32: FGP-1, Liver, PAS, 100x. The intensely red-stained granules present in the cytoplasm of the hepatocytes are glycogen deposits selectively stained by PAS. There is extensive cytoplasmic (cv) and nuclear vacuolization (nv) and the sinusoids appear filled with flocculent cellular debris (d). Indeed, it is only possible to discern the outlines of the original individual hepatocytes from the pattern of the intracellular glycogen granules disclosed by the PAS stain.
Figure 32: FGP-1, Liver, PAS, 100x. The intensely red-stained granules present in the cytoplasm of the hepatocytes are glycogen deposits selectively stained by PAS. There is extensive cytoplasmic (cv) and nuclear vacuolization (nv) and the sinusoids appear filled with flocculent cellular debris (d). Indeed, it is only possible to discern the outlines of the original individual hepatocytes from the pattern of the intracellular glycogen granules disclosed by the PAS stain.